Arachnoiditis
Table of Contents
What is Arachnoiditis?
Arachnoiditis is a condition characterized by inflammation of the arachnoid, which is one of the membranes that surround and protect the nerves of the spinal cord.
Neurological issues and intense stinging, “burning” pain are all symptoms of arachnoiditis. The lumbar (low back) and thoracic (middle back) nerves are most frequently affected. Your entire spine is rarely affected.
Due to the fact that arachnoiditis can either be static (stay the same) or progressive (get worse over time), the course of this sickness is still very unpredictable.
The illness known as arachnoiditis is brought on by arachnoid inflammation. The spinal cord’s nerves are encased and shielded by a number of membranes, including the arachnoid. The following are the causes of arachnoid inflammation:
- the irritation brought caused by chemicals
- infection with viruses or bacteria
- directly causing spinal damage
- spinal nerves are consistently compressed
- complications from spine surgery or other invasive (operations that require rupturing the skin) procedures
- Sometimes, inflammation can result in scar tissue or scar adhesions, which “stick” the spinal nerves together.
Arachnoiditis can result in a variety of symptoms, including chronic and persistent discomfort, numbness, tingling, and a distinctive stinging and burning pain in the lower back or legs if it starts to interfere with the operation of one or more spinal nerves.
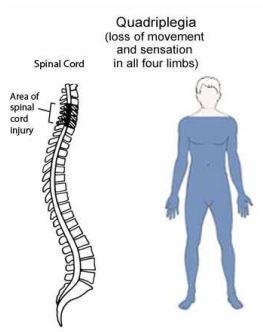
Arachnoiditis can cause some people to have incapacitating muscular cramps, jerks, or spasms. Additionally, it could impair sexual, digestive, and bladder functions. Arachnoiditis can, in severe cases, paralyze the lower limbs.
Treatment for arachnoiditis is still challenging, and long-term results are unclear. The majority of therapies concentrate on reducing chronic pain and symptom severity, which interfere with everyday activities.
Doctors frequently advise patients to combine talk therapy, physical therapy, exercise, and pain management. Surgery for arachnoiditis typically has poor outcomes and only provides temporary relief.
Clinically Relevant Anatomy
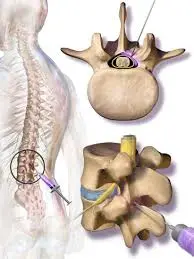
Meninges surround and shield the central nervous system (CNS), which includes the brain and spinal cord. The Dura Mater, which is the outside layer, the Arachnoid Mater, which is the intermediate layer; and the Pia Mater, which is the inner layer, make up the meninges. There are 31 pairs of spinal nerves that leave the vertebral column through the vertebral foramina, one on the right side and the other on the left.
Pathological Process
Arachnoid membrane inflammation causes arachnoiditis, a progressive disease that affects the brain and/or spinal cord. Arachnoiditis comes in a variety of forms, such as adhesive arachnoiditis, which is the most severe type and develops when spinal nerves adhere to one another; arachnoiditis ossificans, which happens when arachnoid tissue transforms into bone, and others. a condition known as cerebral arachnoiditis that damages the brain’s outer membranes, Hereditary arachnoiditis, which is congenital, uncommon, and caused by meningeal anomalies, Neoplastic arachnoiditis, which develops as a result of cancer, and optochiasmatic arachnoiditis, which affects the optic nerve, are three different types of arachnoiditis.
Arachnoiditis has three primary phases.
- The spinal nerve inflammation, hyperemia, removal of the subarachnoid space, and formation of scar tissue are all part of the initial stage.
- The process of creating scar tissue intensifies during the second stage, and the nerves increasingly cling to the dura and one another.
- Complete encapsulation of the nerve roots occurs in the third stage. Compression results in atrophy of the nerve roots, and the scarring tissues stop spinal fluid from being produced in that region. Arachnoiditis Ossificans is a condition in which the scar tissue calcifies.
In arachnoiditis, what occurs to the arachnoid?
The arachnoid mater is one of the three layers of membranes that make up the meninges, which protect and surround your brain and spinal cord (your central nervous system). The arachnoid matrix is the layer in the center. The dura mater and the pia mater are the last two layers.
In the meninges, there are three spaces:
The dura mater covers your skull, the dura mater covers your spinal cord, and the bones of your vertebral column make up the epidural space.
Between your dura mater and arachnoid mater, there may be a region called the subdural space. It can break open if there is a pathological condition, trauma, or a deficiency in CSF fluid that causes the arachnoid mater to split from the dura mater. Arachnoiditis may lead to this.
Your arachnoid mater and pia mater are separated by the subarachnoid space. Cerebrospinal fluid is within. Your brain and spinal cord are cushioned and secured by cerebrospinal fluid.
Your spinal cord’s arachnoid layer, not your brain, is the target of arachnoiditis.
A series of events, including the following, are triggered by injury to and inflammation of the arachnoid (subarachnoid or subdural space) in arachnoiditis.
- collagen accumulating.
- Nerve roots are enclosed by scar tissue.
- Fibrosis (tissue thickening or scarring).
- reduced flow of cerebrospinal fluid.
- root clumping in the nerves.
- reduced blood flow to the injured nerves.
- Nerve wasting or atrophy.
- injury to the nerves, maybe with tethered nerves.
- Arachnoiditis commonly results in discomfort and potential neurological abnormalities, such as muscular weakness and sensory problems, because of these alterations in the arachnoid and nerve roots.
Types of Arachnoiditis
Arachnoiditis is divided into a number of subgroups by doctors. Predicting symptoms can be made easier by understanding the type of arachnoiditis a person has. Various arachnoiditis types include:
- Adhesive arachnoiditis: The most serious and advanced form, this condition develops when the spinal nerves become entrapped together as a result of arachnoid inflammation.
- Arachnoiditis ossificans: This disorder, in which the arachnoid turns into bone, is referred to as arachnoiditis ossificans.
- Cerebral arachnoiditis: The brain membrane is affected by cerebral arachnoiditis, which frequently results in excruciating headaches.
- Hereditary arachnoiditis: This uncommon arachnoiditis is brought on by hereditary meningeal abnormalities.
- Neoplastic arachnoiditis: This term refers to a specific type of arachnoiditis caused by malignancy.
- Optochiasmatic arachnoiditis: Optochiasmatic arachnoiditis is an arachnoiditis of the optic nerve. It might cause severe or complete visual loss.
Causes of Arachnoiditis
Trauma/Surgery-Induced: Arachnoiditis is regarded as an uncommon side effect of spinal surgery, particularly following several difficult procedures or spine trauma. Arachnoiditis can also result from repeated lumbar punctures, severe spinal stenosis, and persistent degenerative disc disease. Inflammation might be brought on by blood entering the subarachnoid space as a result of this.
Myelograms have lately been thought to be the source of this disorder, which is chemically caused. A myelogram is a type of diagnostic procedure that involves injecting a dye into the region that surrounds the spinal cord and nerves. It may be seen in several types of diagnostic imaging, including X-ray, MRI, and CT scans. Arachnoiditis is brought on by often being exposed to the oil-based radiographic contrast materials used in myelograms. It’s also crucial to remember that arachnoiditis brought on by surgery is exactly localized, but arachnoiditis brought on by epidural injections is widespread.
Infection-induced: Meningitis from bacteria or viruses, TB, and syphilis can all impact the spine and result in arachnoiditis.
The third most typical reason for Failed Back Surgery Syndrome (FBSS) is arachnoiditis.
Healthcare professionals frequently are unable to pinpoint the specific causes of arachnoiditis. This is due to the condition’s rarity, various potential origins, and the potential for symptoms to develop sometime following the first episode.
The arachnoid may swell and become irritated by one of the following sources:
- Up to 90% of instances of arachnoiditis have been connected to lumbar spine surgeries, despite the fact that arachnoiditis is an uncommon consequence of these operations. Complications after spinal surgery or numerous lumbar punctures.
- Direct damage to the spine: In a small percentage of instances, direct trauma to the spine, such as from a fall or car accident, can result in arachnoiditis.
Chemicals: Some occurrences of arachnoiditis have been linked to the dye used in myelograms. A radiographic contrast medium dye is injected into the region around your spinal cord and nerves during a myelogram, a diagnostic procedure. However, the iofendylate-based radiography contrast medium that caused this is no longer in use. The risk that the preservatives in epidural steroid injections might cause arachnoiditis is another cause for worry.
Bacterial or viral infection: Arachnoiditis can be brought on by infections including HIV, TB, viral and fungus meningitis, and meningitis.
Arachnoiditis can be brought on by chronic spinal nerve compression, which can be brought on by severe spinal stenosis (narrowing of the spinal column) or degenerative disc degeneration.
Less frequently mentioned arachnoiditis causes include:
- spondylosis with ankylosing.
- the syndrome of Guillain-Barré.
- Vasculitis is caused by autoimmunity.
Symptoms of Arachnoiditis
Persistent discomfort in the lower back and limbs would be the main sign of arachnoiditis. 90% of patients also experience the following additional symptoms:
- The tingling and paresthesia
- a limb weakness in the lower body
- spasms and cramps
- Bladder bowel issues
- hyporeflexia
Although pain is the most typical sign of arachnoiditis, there is no set sequence of symptoms. The severity of the symptoms might range from moderate to severe depending on which spinal nerve (region of your spine) is damaged.
The nerves in your lumbar spine, which attach to your legs and lower back, are most frequently impacted by arachnoiditis.
Numerous signs and symptoms of arachnoiditis include:
- Headaches.
- extreme shooting pain that may seem like an electric shock.
- Leg tingling, numbness, or weakness.
- Feelings that might resemble water trickling down your leg or insects crawling on your skin (formication).
- sitting for lengthy periods of time, if at all.
- cramps, spasms, or involuntary twitching of the muscles.
- bladder with neurogenic characteristics.
- bowel disorder.
- sexual problems, such as dry vagina or erectile dysfunction.
- If the situation worsens, the symptoms can possibly become permanent. Because of the chronic discomfort, many persons with arachnoiditis are unable to work and have a major impairment.
- The pain is typically triggered by non-painful stimuli or no stimulation at all and tends to be worse at night. In contrast to other types of pain, which often startle slowly and continue after physical activity has stopped, this one tends to get worse with exercise. Additionally, because of the spine dynamic modification induced by this illness, pain can also be brought on by reasons other than nerve injury that affect the musculoskeletal system. Patients who have this illness may feel significant joint pain, muscular strain, and an increase in muscle tone owing to nerve injury.
- What is arachnoiditis adhesion?
- As arachnoiditis worsens, it may result in the growth of scar tissue, which will make the spinal nerves clump together and malfunction. Chronic adhesive arachnoiditis is the result of this.
- A disability may result from adhesive arachnoiditis. Due to paraparesis, which happens when you can only move your legs partially, many people with the illness eventually need to use a wheelchair.
- Arachnoiditis is how frequent?
- Though arachnoiditis is uncommon, its exact prevalence is unknown to scientists. Many minor cases of arachnoiditis won’t ever be recognized or won’t be recorded since arachnoiditis can present in a variety of ways, from extremely mild to severe.
- According to recent studies, there seems to be a correlation between the number of lumbar spine procedures and the frequency of lumbar arachnoiditis.
- How dangerous is arachnoiditis?
- Arachnoiditis is rarely life-threatening, but the persistent pain and neurological problems it causes can have a significant impact on your quality of life. For the best care, it’s crucial to locate a medical professional who is knowledgeable about arachnoiditis.
Diagnosis and Tests
Arachnoiditis: How is it identified?
Due to its rarity and the fact that not all medical professionals are familiar with it, arachnoiditis can be challenging to diagnose. Furthermore, there are no conclusive laboratory or imaging test results for the diagnosis of arachnoiditis. The clinical appearance, symptoms, and supporting MRI or CT myelography are used by providers to make the diagnosis.
What examinations will be used to identify arachnoiditis?
The following tests may be prescribed by your doctor if you exhibit signs of arachnoiditis to aid in the diagnosis:
- The procedure of magnetic resonance imaging (MRI), which gives incredibly clear pictures of your body’s organs and structures, is painless. To create detailed pictures, it combines a big magnet, radio waves, and a computer. In an MRI of your spine, your doctor will be looking for specific indicators of arachnoiditis, such as thickening and clumping of the nerve roots.
- Myelogram using computed tomography (CT): A myelogram is a type of imaging test that looks at the connections between your vertebrae and discs by way of your spinal cord, nerves, and nerve roots. Your doctor will be on the lookout for specific arachnoiditis symptoms.
- A lumbar puncture may be necessary if it appears that the cause of arachnoiditis is an infection in the spinal fluid. During this procedure, spinal fluid is removed for testing.
Treatment of Arachnoiditis
Arachnoiditis is a very challenging illness to cure, and the major goals of treatment for people with this condition are to reduce discomfort and improve symptoms that interfere with everyday function.
Sadly, there is no treatment for arachnoiditis. The major goals of treatment are symptom management, pain management, and quality of life improvement.
Arachnoiditis can be treated in a manner similar to other chronic pain problems. Healthcare providers frequently suggest one of the following programs:
- control of pain.
- hydrotherapy and massage are examples of physical therapy.
- range-of-motion exercises and stretching.
- counseling (talk therapy).
- adaptive tools or technologies to improve comfort and mobility.
Particular forms of therapy include:
A spinal cord stimulator is a device that helps to relieve pain by stimulating the spinal cord electrically. Medication: To assist control pain, your healthcare professional can advise using NSAIDs or other stronger drugs. They might also recommend additional medicines like baclofen and muscle relaxants like gabapentin, pregabalin, and duloxetine.
Medical Treatment
The medical treatment plan should concentrate on regulating and suppressing neuroinflammation to stop arachnoiditis from developing and advancing. Non-steroidal anti-inflammatory medicines (NSAIDs) and pulse treatment, particularly methylprednisolone, are frequently used to treat inflammation. Only a small number of trials, nevertheless, have shown that it is beneficial in reducing the production of scar tissue.
Naltrexone, tricyclic antidepressants, and muscle relaxants like baclofen are further pharmaceutical therapies for neuropathic pain. Even if they reduce pain, invasive treatments including intra-spinal narcotic analgesia (INA), epidural steroid injections, and local anesthetic injections are not recommended since they run the risk of escalating the inflammation and making the patient’s condition worse.
Physiotherapy Treatment
The term “Spinal Cord Electrostimulation” (SCS) refers to the electrical stimulation of the spinal cord’s most active pain-producing region utilizing electrodes that have been surgically inserted. When taking into account all forms of chronic pain, some studies suggest a 50% success rate. Patients with arachnoiditis can benefit from a variety of physical therapy techniques, such as heat therapy to ease muscle spasms and LASER therapy to help break down adhesions and reduce inflammation while also calming irritated nerves. Arachnoiditis sufferers need to be treated with extra care, particularly with mild, individually suggested exercises. Regaining mobility, maintaining function, and staying active should be the key priorities. Patients are advised to take daily walks outside of their homes because it is crucial for them to maintain and improve their range of motion in their spine and extremities as much as possible to avoid limitations. This will help them eventually regain their full range of motion, particularly in their arms and legs.
Physiotherapy Treatment is:
- MOIST HEAT: The main purpose of moist heat is to ease muscular spasms.
- SSF: By decreasing spasms and boosting the blood flow to the region, SSF also eases pain. When nerve roots are involved and there is radiating pain, TENS may be used to treat the patient. TENS is frequently utilized, even in paresthesia instances.
- LASER: Laser therapy has been shown to ease the pain of patients by reducing inflammation and releasing adhesions in deep-seated structures that are causing irritation to the patient’s nerve roots.
- Active exercises: Active exercises, such as static workouts for the quadriceps, gluteus, back extensor, and abdominus, serve to reduce discomfort in the early stages and also maintain muscle tone.
- Dynamic exercises: Once the patient’s tolerance for discomfort has been reached, dynamic exercises may be begun. The patient may maintain these activities for the rest of their lives in an effort to reduce the likelihood of a recurrence.
- SLR: Both active and passive SLR are used to stretch and relax the neuronal structures. This particular form of neural mobilization aids in reducing the symptoms of radiculopathy.
- Gait training: In situations of muscle weakness
Psychological support
Chronic pain may make daily life challenging. By altering how individuals perceive their suffering and providing them with emotional support, therapy can help some people manage.
Support groups for those with chronic pain or uncommon conditions can also be helpful to some people. People in pain may uncover new resources, discuss practical lifestyle treatments, and feel less alone with the aid of these communities.
Substitute treatments
Alternative treatments including acupuncture, dietary and lifestyle modifications, or homeopathy can provide relief for some people.
More research is required to ascertain the efficacy of complementary therapies in treating arachnoiditis symptoms.
Surgical Treatment
The surgical procedure primarily aims to remove cicatricial adhesions and restore CSF flow. Because it adds extra scar tissue and stress to the already inflamed spinal cord, its effects are short-term and only temporarily relieve the symptoms experienced by people with this illness.
Differential Diagnosis
The patient’s past medical history, physical tests, and radiographic testing are the key components of the clinical diagnosis of arachnoiditis. The clinical characteristics of arachnoiditis are mimicked by a number of illnesses, including tumors and infections of the spinal cord, its roots, and its plexus. An MRI of the lumbar spine should be performed in addition to screening lab tests to evaluate the complete blood count, erythrocyte sedimentation rate, and anti-nuclear antibody testing in order to rule out the potential for other illnesses. If there is any doubt about the arachnoiditis diagnosis, these tests should always be carried out.
Prevention
Unfortunately, arachnoiditis cannot currently be prevented.
Prognosis
Arachnoiditis may be progressive, meaning it becomes worse with time, and is often chronic (lifelong). There is no cure, however, therapies and treatments can help control symptoms.
Due to severe neurological symptoms and discomfort, persons with severe arachnoiditis frequently have a poor quality of life.
Some individuals with arachnoiditis may develop a handicap and be unable to work a full-time job as a result of ongoing discomfort and numerous neurological problems. But many persons with arachnoiditis are able to walk and operate a vehicle with very minor restrictions.
When I have arachnoiditis, how can I care for myself?
It’s crucial to take care of yourself in addition according to your healthcare provider’s strategy for managing your symptoms, which may include medication and counseling. You may better your general health and manage chronic pain by doing the following actions:
- Don’t smoke.
- Try not to take on too much. Make a daily routine with a few priorities, downtime, and time for self-care.
- Adopt a balanced diet.
- If you can, try to exercise frequently.
- Get adequate rest.
- Maintain stress control.
- To learn from others who have comparable diseases, consider joining a support group for chronic pain or arachnoiditis.
- Alcohol should be used in moderation since it might worsen discomfort and sleep issues.
- Consider thinking optimistically.
- Use pain-relieving techniques including meditation, aromatherapy, biofeedback, and mindfulness exercises.
- It’s crucial to get therapy for your mental health issue(s) if you suffer from both chronic pain and depression, anxiety, or both. Experiencing chronic pain might get worse if you’re depressed or anxious. For instance, weariness, altered sleep patterns, and decreased activity may make your chronic pain worse if you have depression.
FAQs
Arachnoiditis may result in symptoms including tingling, numbness, and a distinctive stinging and burning pain in the legs or lower back if it interferes with the nerves’ ability to operate. It may interfere with certain people’s sexual, digestive, and bladder functions. The legs may become paralyzed in cases of really severe arachnoiditis.
Although there is no recognized therapy for this illness, there are options for pain management. Although non-invasive therapies like physical therapy and painkillers may be utilized at first, arachnoiditis often does not react well to these types of treatments.
The spinal nerve inflammation, hyperemia, removal of the subarachnoid space, and formation of scar tissue are all part of the initial stage. The process of creating scar tissue intensifies during the second stage, and the nerves increasingly cling to the dura and one another.
Arachnoiditis is a condition brought on by arachnoid inflammation. One of the membranes that envelop and shield the spinal cord’s nerves is the arachnoid. Inflammation of the arachnoid can result from Chemical irritation.
Practice Essentials for Radiography with Arachnoiditis…
Magnetic resonance imaging (MRI) is the method of choice for the diagnostic assessment of arachnoiditis due to its noninvasive nature, multiplanar capabilities, and excellent soft-tissue characterization. Computed tomography (CT) myelography is a suitable option for patients in whom MRI is contraindicated.
A chronic infection, chemical reaction, or mechanical stress can cause arachnoiditis, an inflammation of the arachnoid mater and subarachnoid space. Some medical professionals may not fully comprehend this uncommon yet dangerous illness. Adhesive arachnoiditis has the potential to be an extremely painful and incapacitating illness in its most severe form.
Exercises are crucial for preventing the clumping, scarring, and adhesion formation of spinal nerve roots, which can result in paralysis and/or paraparesis of the lower extremities. The warning is clear: either keep moving or risk paralysis. We instruct patients on the benefits of daily stretching for their upper and lower extremities.
Patients with Adhesive Arachnoiditis can receive precise treatment without general anesthesia with less tissue damage, decreased risk, and improved long-term outcomes with a single, carefully focused operation.
Arachnoiditis can cause the meninges to become severely scarred, which can result in a crippling, ongoing searing sensation that is typically accompanied by acute, stabbing pains. Although it mostly affects the lower back and limbs, it can also go up the spine and up the arms.
According to the National Organization for Uncommon Disorders, arachnoiditis is regarded as an uncommon disease that affects around 11,000 individuals annually in the United States, while it is probably underdiagnosed. It almost invariably results from a medical operation, and there is no known treatment for it.
Patients with arachnoiditis are often treated by a specialist in chronic pain. This specialist may have training in internal medicine, occupational medicine, or physical medicine, among other specializations. Some individuals’ symptoms can be lessened with a spinal cord stimulator that can be surgically implanted.
Spinal cord stimulation (SCS) and intrathecal infusion of the N-type calcium channel blocker ziconotide are two separate treatments that can significantly reduce chronic pain from various causes in people with arachnoiditis.
The success rate in other series, was roughly: Failure rates were 50%, 20% could work but had symptoms, and 10% to 19% had no symptoms. The surgical procedure involves removing the extradural scar that surrounds the thecal sac, extracting any disc segments that have herniated, and, if necessary, executing foraminotomies.
Arachnoiditis symptoms don’t follow a predictable pattern. When there are few obvious signs, the illness may occasionally be subclinical. Even while the illness is rarely thought to be life-threatening, at other times it can be crippling.
illnesses brought on by bacteria, viruses, fungi, or parasites that progress to the brain or spinal cord.
illnesses that impair immunity, such as diabetes, AIDS, alcoholism, and organ transplantation.
surgery-related complications involving the spine or brain.