Spinal Muscular Atrophy (SMA)
Table of Contents
What is a Spinal Muscular Atrophy?
Spinal muscular atrophy is an inherited disease in which progressive muscle weakness and wasting (atrophy) are used for movement (skeletal muscles). It occurs due to a loss of specialized nerve cells (motor neurons) that control muscle movement.
Progressive muscle weakness is seen as more severe that is closer to the center of the body as compared to muscles away from the body’s center (distal part of the body). Muscle weakness mostly increases with age. There are various types of spinal muscular atrophy that are occurs by changes in the genes.
Spinal Muscular Atrophy (SMA) is a genetic condition underneath the scope of neurodegenerative disorders and motor neuron disease MND. It is distinguished by the degeneration of alpha motor neurons in the spinal cord that affects the control of voluntary muscle movement.
The disease is distinguished as an autosomal recessive condition with a prevalence of approximately one in 6-10,000 births affected by SMA with a carrier frequency of one in 35-70. Classification of SMA type based on the age of onset and the highest level of motor function achieved.
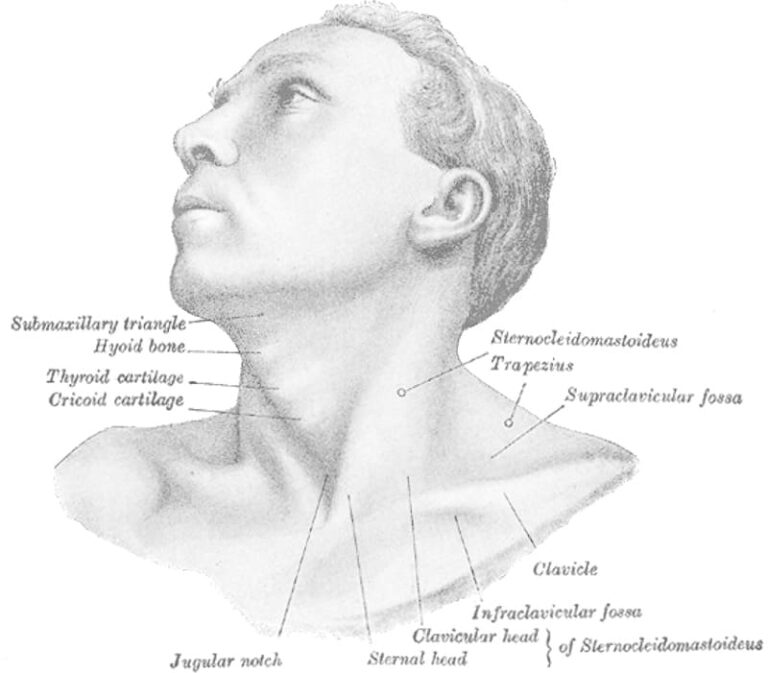
Clinically Relevant Anatomy
- SMA is caused by a deficiency of a motor neuron protein known as SMN (Survival Motor Neuron).
- This protein is important for normal motor function and the lack of it is caused by genetic flaws in chromosome five in the gene SMN1.
- The neighboring SMN2 gene may compensate for some of the functions of SMN1 and this is where some pharmaceutical companies try to generate a drug that may improve the effect of SMN2.
Pathological Process
- Spinal Muscular Atrophy is an autosomal recessive condition in most cases to the homozygous deletion of the SMN1 gene.
- This means that both parents of the affected people are the only carriers of the affected gene.
- Therefore, they are not going to present with any kind of symptoms of the disease and this is what makes SMA difficult to foresee and apply preventable measures.
Signs and Classification of Spinal muscular atrophy
- Spinal Muscular Atrophy (SMA) is the 2nd most usual neuromuscular disorder in childhood.
- Individuals affected by the mildest types of SMA have proximal weakness and impaired ambulation.
- Moreover, fatigue is a symptom present in almost every case of SMA which can also lead to impaired function and endurance.
- Recent research in the area shows that there is a good connection between upper and lower limb function in people with the disease.
- There are too many types of SMA, which begins at different ages and can come with various phenotype.
Types of SMA
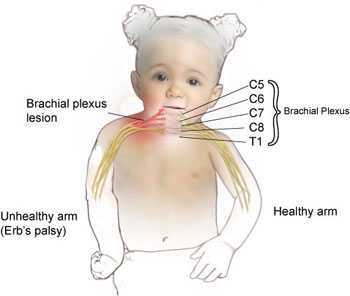
SMA type I (Werdnig-Hoffmann disease) –
- Affects children less than 6 months old and is the most severe type of the disease.
- Sitting unsupported can never be achieved.
- Comes with profound hypotonia, symmetrical flaccid paralysis, and no head control with poor spontaneous mobility and reduced antigravity movements of limbs.
SMA type II-
- Generates in children between seven and eighteen months old.
- This form is less severe than type one and most babies survive into adulthood and may live long, fulfilling lives.
- Can achieve the ability to sit without any kind of support but can not be able to walk separately.
- Joint contractures and kyphoscoliosis are very usual along with fine tremors of the upper extremities.
SMA type III (Kugelberg-Welander disease) –
- Comes after eighteen months of age and is the least common type affecting babies.
- SMA type III has been divided into 2 further sub-categories:
- SMA IIIa and SMA IIIb – according to the time when the 1st symptoms of the condition appear (if before or after three years of age).
SMA type IV –
- This form of SMA patients are diagnosed in adulthood and they come with only mild problems.
Diagnostic Procedures
- Diagnoses may be made by prenatal screening or by gene panel investigation and/or muscle biopsy.
- In the initial stages, the diagnosis can be suspected because of symptoms such as floppiness and muscular weakness.
- Children with type one SMA may come with a lack of head control, minimal to absent anti-gravity movements, and severe respiratory complications.
- The 1st step in diagnosing someone with SMA will be by taking a full clinical examination and family history.
- A blood test can be needed to look at the amount of creatine kinase (CK), and an investigation to identify if muscle damage has occurred.
- High levels of CK in the blood are not damaging themselves, but it is a necessary indicator of a muscle disorder condition.
- Electrophysiological tests like electromyography (EMG), and nerve conduction study should be done, if EMG indicates a motor neuron disease, then, further testing should be done.
- Too many other investigations will probably involve genetic testing as this is the most perfect way to diagnose if a person has Spinal Muscular Atrophy.
Outcome Measures
There are too many other outcome measures that may be used to find the changes in the natural history of patients with SMA. These tools should be estimated and selected according to the age and severity of the disease.
Six-Minute Walking Test (6MWT) –
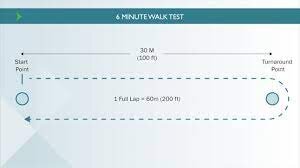
- The Six-Minute-Walking-Test may be safely performed in an ambulant person with SMA.
- It has been proven to find out fatigue-related changes in this population of patients and also correlates with other established outcome measures for people with spinal muscular atrophy.
Revised Hammersmith Scale for SMA (RHS) –
- The RHS is predominantly utilized in patients with SMA types two and three.
- In a combination with the WHO motor milestones, the scale may be more sensitive toward the description of the SMA phenotype.
- The RHS has been planned to apprehend a huge range of abilities across a broad spectrum of SMA, from very young babies to adolescents and adults.
Differential Diagnosis
Neuromuscular conditions:
- Duchenne Muscular Dystrophy (DMD)
- Charcot-Marie-Tooth
- Amyotrophic Lateral Sclerosis
Congenital Myopathies:
- Congenital myotonic dystrophy,
- Congenital myasthenic syndromes,
- Metabolic myopathies
- Congenital disorders of the motor neuron and the peripheral nerve (congenital hypomyelinating neuropathy).
Non-Neuromuscular Conditions:
- Prader-Willi syndrome,
- Acute hypoxic-ischemic encephalopathy,
- Neonatal sepsis and
- Dyskinetic or metabolic conditions
- The tools that may identify these differential diagnostic possibilities beyond the clinical examination and careful family history are CK determination, EMG/nerve conduction studies, MRI of the brain, muscle biopsy, and specific genetic or metabolic testing.
Treatment of Spinal muscular atrophy
- Spinal Muscular Atrophy (SMA) is a severe genetic condition that needs precise diagnosis and extensive physiotherapy treatment in order to protect the muscles from quick deterioration and development of contractures.
- The management of SMA must be as a part of a large multi-disciplinary team which should involve rehabilitation, spinal management, orthopedics, nutritional and gastrointestinal management.
- Currently, it has been stated that SMA can be a multi-organ disease and a more detailed examination should be done.
- Further suggestions have been made on pulmonary management and acute care issues in the severe kind of spinal muscular atrophy.
Medical Management:
- Neuroprotective Drugs such as riluzole,
- Drugs to improve energy metabolism and
- Drugs affecting the gene expression of SMN
Gene Therapy:
- Along with advances in medical management, gene therapy approaches have been suggested for SMA, using viral vectors to replace SMN1 gene.
Stem Cell Therapy:
- Cellular replacement strategy in the rehabilitation of SMA.
- However, this therapy is still in the research stages.
Cell replacement can be achieved by :
- Transplantation of stem cell-derived cells that have undergone maturation in vitro.
- Activation of endogenous stem cells in the CNS
Physiotherapy Treatment in Spinal muscular atrophy
Assessment of the person with neuromuscular disease and specifically with SMA is of great importance. Looking at baseline function, joint range and power will assist the physiotherapist to follow the recovery stage of the condition.
- Orthotics
- Splinting
- Taping
- Management of contractures
- Exercise and activity
Respiratory Care
- Many babies and adults with Spinal Muscular Atrophy will be dependent on pulmonary management because of loss of muscle function.
- When a patient with SMA has a respiratory failure they require to be transferred on non-invasive positive pressure ventilation (NIV).
- In order for this to be implemented in the best possible way, a respiratory physiotherapist should be included in the assessment and management of pulmonary complications.
- Airway clearance (chest physio) is best administered with the combination of Cough Assist and this should be the initial airway clearance therapy for all SMA patients with respiratory illness.
- Suctioning is a critical part of the treatment and should be utilized in all patients with excessive secretions or in those with ineffective cough.
- The high-frequency chest wall oscillation (Vest) is another great option for managing secretions.
- However, there is no evidence that the Vest increase airway clearance and secretions.
- Non-invasive positive pressure ventilation (NIV) should be utilized for respiratory failure or to prevent chest wall distortion.
- Continuous positive airway pressure (CPAP) should be utilized only when NIV is not tolerated or in the treatment of chronic respiratory failure.
Physical therapy treatment for individuals with SMA can involve activities to:
Maintain and increase overall movement and function. This involves improving developmental skills in infants and children like:
- Head and trunk control.
- Rolling.
- Crawling.
- Sitting.
Changing positions
- The child’s physical therapist will work on skills such as getting in and out of bed or pulling to stand.
- They also can work with the child on balance and coordination for more advanced skills like going up and down stairs and walking.
- Prevent or less the progression of muscle shortening (tightness), stiffness, and joint deformities.
- Physical therapists help the person to learn specific flexibility and range-of-motion exercises and positioning.
- They also may recommend splints, braces, standing devices, or serial casting (to reshape deformed limbs or joints).
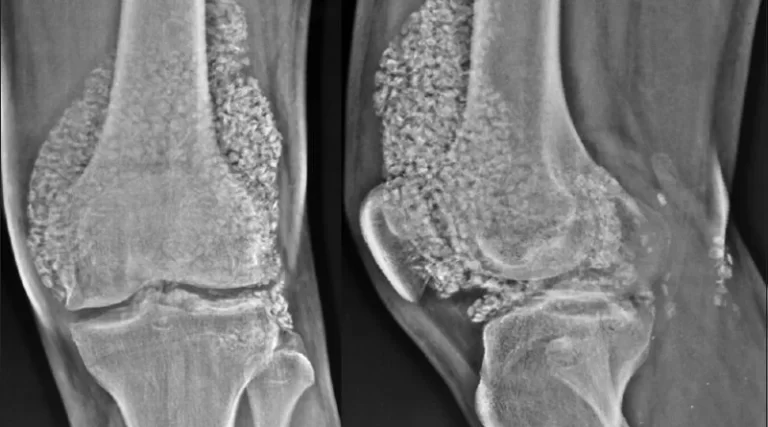
Manage scoliosis and bone problems
- Physical therapists work with individuals to help keep up the spine and body supported and aligned at the time of daily activities.
- They design treatment programs and can use braces or supportive seating to help individuals with SMA maintain good posture and protect their bones and joints.
- If scoliosis or other joint problems caused by SMA needs surgery, physical therapy can be provided before and after surgery.
Manage breathing complications
- Respiratory exercise training is important for individuals with SMA to prevent breathing problems.
- It also is also important before and after surgery. Physical therapists learn the parent’s and caregivers’ methods for chest drainage.
- They also help a person and the child learn how to clear the chest and teach coughing and breathing practices to keep up the lungs free of fluids so they may breathe well.
- Chest physical therapy also involves core and breathing exercises and postural support through good positioning.
- They also suggest custom and molded wheelchair seating systems and custom sleeping systems.
Select assistive devices
- Many individuals with SMA require adaptive or assistive devices to help them function, specifically after surgery.
- Physical therapists work with other specialists to select and modify suitable devices to meet every individual’s requirements.
- Physical therapists teach patients and caregivers how to safely use assistive devices to help individuals with SMA eat, play, move, communicate, or work.
- Assistive devices to support positioning and movement can involve strollers, wheelchairs, customized seating systems, walkers, and standers.
- These devices help individuals with SMA be as independent and mobile as possible.
Strengthen muscles and maintain aerobic fitness
- Exercise can help to increase aerobic fitness in individuals with SMA.
- Physical therapists select the perfect type and intensity of exercises to help individuals with SMA move and stay as active as possible.
Improve function during mealtime
- Physical therapists work nearly with speech and occupational therapists to give healthy feeding.
- They teach a person how to align and support the child’s head and body for safe eating and meal enjoyment.
- They also can teach a person ways to help to chew and swallow.
- Because of problems swallowing, many children with SMA are on specific diets under the guidance of a registered dietician.
- To ensure that they get enough calories and balanced nutrition, some individuals with SMA receive their feedings through tubes (either through the nose or a surgically put feeding tube).
- Others needed tube feedings to add to their food intake.
- Therefore, therapists and families must receive clearance from the child’s doctor prior to working on feeding.
- The child’s physical therapist will select exercises, games, and fun tasks that will be taught at the time of therapy.
- They also teach families positioning and activities to help increase everyday habits at home.
- Physical therapists rigorously monitor exercise and activity levels to avoid fatigue.
- They help patients and families understand how to decrease the risk of overworking muscles.
Aquatic therapy or hydrotherapy (therapy given in a pool)
- They utilize the physical properties of water (like buoyancy and pressure) to decrease the risk of fatigue or overworked muscles.
- The buoyancy and reduced gravity in water allow individuals with SMA to move, stand, and walk more easily than they can on land.
- The water’s support may enable strengthening, balance training, and aerobic training.
- Some non-sitters may be part of it safely in aquatic therapy with proper head and neck support and supervision.
Physiotherapist’s role before and after the surgery
- Individuals with SMA can require surgery for scoliosis, hip alignment, or to release joint tightness.
- A physical therapist will evaluate a person or the child before any scheduled surgery.
- They will plan for the equipment required and design a treatment program after surgery.
- Early movement after surgery is frequently suggested, so developing a plan of action prior to surgery is important.
- Physical therapists also will see the person or the child again shortly after surgery.
- Resuming physical therapy as early as possible helps keep comfort, and muscle strength, and gives education for after-surgery care.
- Physical therapists also give traditional movement plans for the early treatment phase after surgery.
- Longer-term physical therapy permit for continued improvements in function and mobility after surgery.
FAQ
Infants with type 1 SMA generally die prior to their second birthday. Children with type two or type three SMA can live full lives depending on the severity of their symptoms. Individuals who develop SMA at the time of adulthood (type 4) frequently remain active and enjoy a normal life expectancy.
If a woman is pregnant and there is a risk that a female could have a child with SMA, tests may be carried out to check for the condition. The two main tests are: chorionic villus sampling (CVS) – a sample of cells from the placenta are tested, generally during weeks 11 to 14 of pregnancy.
Most of the Body tissues and organs are intrinsically (and independently) affected by Spinal Muscular Atrophy (SMA). Sex plays a vital role in diagnosing the overall prevalence and severity of SMA. Male reproductive body part development and male fertility are adversely impacted in SMA.
Spinal muscular atrophy (SMA) refers to a group of hereditary diseases that may damage and kill specialized nerve cells in the brain and spinal cord (motor neurons).
Conservative primary treatment is suggested in all patients with superior mesenteric artery syndrome; this involves adequate nutrition, nasogastric decompression, and proper positioning of the patient after eating (ie, left lateral decubitus, prone, knee-to-chest position, or Goldthwaite maneuver).




2 Comments