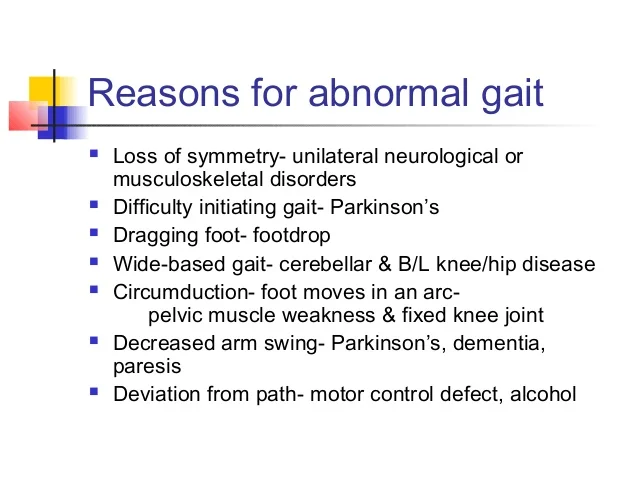
List Of Abnormal Gait: Physiotherapy Treatment:
Following are the list of Abnormal Gait:
1) Hemiplegic Gait
2) Diplegic Gait
3) Neuropathic Gait
4) Ataxic Gait
5) Parkinsonian Gait
6) Sensory Gait
8) Myopathic Gait
9) Scissor gait
10) Hyperkinetic gait
11) Propulsive gait
12) Trendelenburg gait
13) circumductory gait
14) Choreiform Gait
15) Wadlling gait
16) High stapping gait
(1) HEMIPLEGIC GAIT :
Unilateral weakness Leg extended with plantar flexion Circumduction due to the weakness of the distal muscles, equinus foot and extension hypertrophy of the lower limb
Physiotherapy Treatment :
- preventing adaptive changes in lower limb soft tissues
- eliciting voluntary activation in key muscle groups in lower limbs
- increasing muscle strength and coordination
-increasing walking velocity and endurance - maximizing skill, i.e., increasing flexibility
- increasing cardiovasular fitness
- Range Of Motion (ROM) Exercises
- Muscle Strengthening Exercises
- Mobilization activities
- Fitness training
- Compensatory Techniques
-force exercise, reduction of spasticity, gait symmetry, utilization of equilibrium reflexes, stepping automation, endurance training, repetition of rhythmic movements - treadmill training, with partial body-weight support, locomotor pharmacotherapy, selective reduction of spasticity by botulinum toxin injections, and by musical biofeedback, which have each proved to be successful in the restoration of gait pattern.
- Treadmill training based on partial body weight support, combined with enforced stepping movements has proved to be successful in the restoration of gait pattern.
- an ankle-foot orthosis (AFO) is the appropriate technical aid.
- botulinum toxin injection into spastic leg muscles has been successfully used to improve gait functions.
- auditory (musical) rhythm, as a peripheral pacing signal, resulted in a significant increase in weight-bearing stance time on the paretic side.
(2) DIPLEGIC GAIT:
-Patients have involvement on both sides with spasticity in lower extremities worse than upper extremities.
-The patient walks with an abnormally narrow base, dragging both legs and scraping the toes.
-This gait is seen in bilateral periventricular lesions, such as those seen in cerebral palsy.
-There is also characteristic extreme tightness of hip adductors which can cause legs to cross the midline referred to as a scissors gait.
Physiotherapy :
- The functional stretching exercises were performed by training the child to maintain walk standing and stride standing positions with gradual increase of distance between lower limbs with extended knees to stretch lower limb muscle, and the child was trained to stoop and recover from these positions
-The child was trained to walk with full extended knees and hips in slight abduction with correction of lower limb rotation - Strengthening of abdominal and back muscles was performed with hip joint abductions and knee joint extension
- The child may need a walker, braces and other forms of mobility assistance. In some cases, surgery is indicated when there is increased pain or limb deformities.
-Many parents are taking their children to massage and yoga therapy, which helps relax muscles via deep massage and builds strength. Talk to your child’s doctor if you think massage therapy or yoga might be a good choice for your child
-effective therapies include aqua therapy, using recip- rocal movement of the lower extremities,s7 and therapeutic horseback riding.
-The therapist also should emphasize active trunk ex- tension and increased trunk and pelvic mobility. which can lead to improved posture and balance
- Static magnetic field therapy
- Low-intensive laser therapy
- Monochromatic infrared light
- Specific exercise programme including range of motion, muscle strengthens and gait training can improve gait pattern or walking in patients with diabetic neuropathy. Evidence shows that resistant strengthening exercises lower blood glucose level
- (4) ATAXIC GAIT:
- Most commonly seen in cerebellar disease, this gait is described as clumsy, staggering movements with a wide-based gait. – While standing still, the patient’s body may swagger back and forth and from side to side, known as titubation. – Patients will not be able to walk from heel to toe or in a straight line. – The gait of acute alcohol intoxication will resemble the gait of cerebellar disease. – Patients with more truncal instability are more likely to have midline cerebellar disease at the vermis.
- physiotherapy Treatment:
- Require coordinated movement of small muscles (hands, face).
Examples: include writing, drawing, buttoning a shirt, blowing bubbles - Require coordinated movement of large muscles or groups of muscles (trunk, extremities).
Examples: include walking, running, lifting activities. - Frenkel’s exercises
Proprioceptive Neuromuscular Facilitation
Neurophysiological Basis of Developmental techniques
Sensory Integrative Therapy - Standing in a normal comfortable posture.
Standing with feet together (narrow base of support)
Standing with one foot exactly in front of the other in tendon (toe of one foot touching heed of opposite foot).
Standing on one foot. - Standing and then alternate between forward trunk flexion and return to neutral.
Standing with trunk laterally flexed to each side.
Standing to test the ability to maintain an upright posture without visual feedback.
Standing in tandem position from eyes open to eyes closed - Stabilizing the trunk and proximal muscles should begin with mat activities such as moving onto the forearms from lying face down; crawling; and moving onto the knees and into a sitting position.
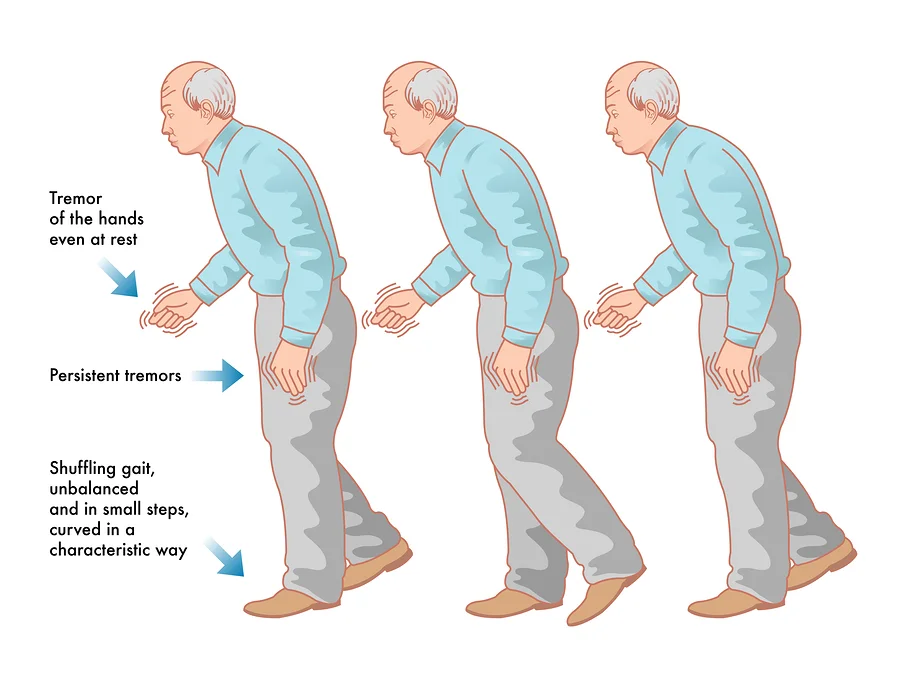
- (5) PARKISONIAN GAIT:
- In this gait, the patient will have rigidity and bradykinesia. – He or she will be stooped with the head and neck forward, with flexion at the knees. – The whole upper extremity is also in flexion with the fingers usually extended. – The patient walks with slow little steps known at marche a petits pas (walk of little steps). – Patient may also have difficulty initiating steps. – The patient may show an involuntary inclination to take accelerating steps, known as festination. – This gait is seen in Parkinson’s disease or any other condition causing parkinsonism, such as side effects from drugs.Physiotherapy Treatment :The training focused on stretching, improving balance and range of movements, thrice a week for six monthsexercise training improves aerobic capacities, muscle strength, walking, posture and balance parameters.Rehabilitation programs should begin as soon as possible, last several weeks and be repeated. They should include aerobic training on bicycle or treadmill and a muscle strengthening programeffect of exercise training by using the Nintendo Wii Fit video game and balance board system on balance and gait in adults with PD.Attentional strategies are consciously concentrating on a specific aspect of gait.effects of an aquatic-based physical exercise program on gait parameters of patients with PD.significant improvement in walking speed, stride length and on the relationship between single and double support timeTreadmill training can be expected to result in improvements in gait speed, stride length and walking distance.The maintenance of cadence following treadmill training, in conjunction with increased stride length, results in faster gait speed which is a positive outcome
- (6)SENSORY GAIT: The sensory ataxic gait occurs when there is loss of this propioreceptive input. – In an effort to know when the feet land and their location, the patient will slam the foot hard onto the ground in order to sense it -this gait involves its exacerbation when patients cannot see their feet (i.e. in the dark). – This gait is also sometimes referred to as a stomping gait since patients may lift their legs very high to hit the ground hard.
- Physiotherapy: improve balance and increase the independence of the patient using techniques focusing on balance, posture and increasing coordination.Therapeutic goals include improving balance and posture against outside stimuli, increasing joint stabilization, developing independent, functional gait to promote independenceTraining principles include progressing from simple to complex exercises, practicing exercises with eyes open and closed and providing support with home exercise and sports activitiesStabilizing the trunk and proximal muscles should begin with mat activities such as moving onto the forearms from lying face down; crawling; and moving onto the knees and into a sitting position.Therapy involves plyometric exercises, balance board and mini trampoline exercises. Yoga and other body-awareness exercises may also be included in the treatment plan to increase proprioception.one leg at the hip and knee with the heel raised from the bed. Straighten your leg to return to the starting position. Repeat with the other leg.make two cross marks on the floor with chalk. Alternately glide the foot over the marked cross: forward, backward, left and right.walk forward placing each foot on a footprint traced on the floor. Foot prints should Learn to rise from the chair, at two, bend trunk forward; at three, rise by straightening the hips and knees and then the trunk. Reverse the procedure to sit down.larn to rise from the chair, at two, bend trunk forward; at three, rise by straightening the hips and knees and then the trunk. Reverse the procedure to sit down.
- (8) MYOPATHIC GAIT: Hip girdle muscles are responsible for keeping the pelvis level when walking. – If you have weakness on one side, this will lead to a drop in the pelvis on the contralateral side of the pelvis while walking With bilateral weakness, you will have dropping of the pelvis on both sides during walking leading to waddling. – This gait is seen in patient with myopathies, such as muscular dystrophy. physiotherapy:
- stretching and strengthening programmes to help maintain muscle strength and flexibility.
- increased muscle strength
- increased balance
- increased flexibility
- reduced risk of falls
- Range of motion exercises are important in maintaining joint function and muscular balance and may play a role in reducing pain that is caused by muscular imbalance or tightness
- yoga and Pilates based activities that can either be done individually or in a class setting.
- Strengthening exercises may help to minimize the disuse weakness; but there is also a concern that too much exercise or inappropriate exercise may hasten disease progression, and hence finding the right balance for each individual is important.
- Strengthening exercise can be accomplished in several ways with resistance provided by gravity, water – in a pool – or equipment such as elastic bands, free weights and machines.
- Yoga and Pilates types of exercises may also be recommended as part of a strengtheninsg program
- (9) SCISSOR GAIT:
- Caused by hip adductor spasticity -Most evident during swing phase -The trunk may lean over the stance leg as the swing leg attempts to swing past it.
- physiotherapy:
- To improve muscle power:
Electrical stimulation
Strengthening exercise of weak group of muscle by resisted exercise
Strengthening of knee extensor muscle helps to improve stride length
Aquatic therapy
- To prevent contractures to reduce spasticity:
To reduce the flexed postures of the body the patient should be advice to lying in prone position
Encourage to sit near the corner side of hall it will reduce the spasticity of muscle and helping the child to sit in correct position
Proper relaxation positioning
Active ROM exercise of the entire joint
Gentle stretching to increase the ROM - Gait and balance training:
First make the patient to walk with support on even surface and the progress to an uneven surface
Improve the heel to toe gait pattern
Improve side stepping
Increase the BOS during walking and progress from wide to narrow BOS
It should be noticed while the leg is kept slightly apart from each other. - (10) HYPERKINETIC GAIT:
- This gait is seen with certain basal ganglia disorders including Sydenham’s chorea, Huntington’s Disease and other forms of chorea, athetosis or dystonia. The patient will display irregular, jerky, involuntary movements in all extremities -Walking may accentuate their baseline movement disorder. physiotherapy:- -Proximal stability training involved core strengthening exercises with the inclusion of cues that guided the patient’s attention to increasing awareness of his body in space during activities such as weighted trunk rotation
- Balance training involved progressively reaching his limits of stability during activities in a standing position such as reactive stepping. Functional movement training involved increasing body awareness during functional movement patterns such as multi-directional gait training.Medicines (muscle relaxers, anti-spasticity medicines) can reduce muscle overactivity.Get enough rest. Fatigue can often cause a person to stub a toe and fall.effective therapies include aqua therapy, using the reciprocal movement of the lower extremities,s7 and therapeutic horseback riding.
-The therapist also should emphasize active trunk extension and increased trunk and pelvic mobility. which can lead to improved posture and balance((11) PROPULSIVE GAIT:Propulsive gait is when a person walks with his or her head and neck pushed forward. It can appear as though the person is rigidly holding a slouched position.
– physiotherapy:-Correct the abnormal posture by positioning or by using splint to prevent deformity
Stretching of the contracted muscles: to reduce the spasticity
Strengthening exercises may help to minimize the disuse weakness; but there is also a concern that too much exercise or inappropriate exercise may hasten disease progression, and hence finding the right balance for each individual is importantRange of motion exercises are important in maintaining joint function and muscular balance and may play a role in reducing pain that is caused by muscular imbalance or tightness
- Encourage the person to be as independent as possible.
- Allow plenty of time for daily activities, especially walking. People with this problem are likely to fall because they have poor balance and are always trying to catch up.
- Provide walking assistance for safety reasons, especially on uneven ground.
- See a physical therapist for exercise therapy and walking retraining.
- Leg braces and in-shoe splints can help keep the foot in the right position for standing and walking. A physical therapist can supply these and provide exercise therapy, if needed.
- Medicines (muscle relaxers, anti-spasticity medicines) can reduce muscle overactivity.
- Get enough rest. Fatigue can often cause a person to stub a toe and fall. (
- (12) TREDLENBERG GAIT:- Trendelenburg gait occurs when a patient has paralysis/paresis of the hip abductors. -Hip abductor weakness may be caused due to neuronal injury to the superior gluteal nerve either due to nerve entrapment or by iatrogenic factors.
-Trendelenburg gait is also observed in patients with developmental dysplasia of the hip, congenital dislocation of the hip (CDH), congenital coxa vara, or coxa valga secondary to other disorders like Legg-Calvé-Perthes disease or slipped capital femoral epiphysis. - physiotherapy treatment:-
- -An appropriate exercise to strengthen the hip abductors is to have the patient lie in side-lying on the unaffected side and abduct the upper leg towards the ceiling
- To make the exercise more challenging, a weight or theraband can be placed around the active limb.
- Other exercises in the treatment of Trendelenburg gait include functional closed-chain exercises, lateral step-ups and functional balance exercises
- It is also important to strengthen the rest of the hip muscles on the affected side
- Patients with trendelenburg suffer from abnormal range of motion in hip and trunk; so, a wall mirror biofeedback could also be used
-This treatment is used to increase the hip and trunk range of motion
-therapists watches and gives advise/correction to posture, so as to facilitate proper gait re-education - (13) CIRCUMDUCTORY GAIT:
- Patients with a circumduction gait are unable to achieve adequate clearance for the foot to move through the swing phase on the affected side. – To compensate, the patient abducts her thigh and swings her leg in a semi-circle to attain adequate clearance. There are many possible causes, including difficulty with hip flexion, knee flexion, or ankle dorsiflexionpossible causes, including difficulty with hip flexion, knee flexion, or ankle dorsiflexion physiotherapy:
- Balance training involved progressively reaching his limits of stability during activities in a standing position such as reactive stepping. Functional movement training involved increasing body awareness during functional movement patterns such as multi-directional gait training.Medicines (muscle relaxers, anti-spasticity medicines) can reduce muscle overactivity.Get enough rest. Fatigue can often cause a person to stub a toe and fall.effective therapies include aqua therapy, using the reciprocal movement of the lower extremities,s7 and therapeutic horseback riding.
- Increase muscle strength and coordination in the lower limbs
- Retrain voluntary response in the lower muscle groups
- Increase flexibility, cardiovascular fitness, and balance
- Proper gait starts with your feet. You need the ability to strike the ground with your heel, follow through, and push off your toes.
- ankle Dorsiflexion (Passive)
- Seated Marching
- Heel Raises (Active)
- Assisted Toe Raises (Passive)
- Toe Taps
-Toe Taps - Flamingo Stands -Side Leg Raises
- (14) CHOREIFORM GAIT:
- Basal ganglia disease refers to a group of physical dysfunctions that occur when the group of nuclei in the brain known as the basal ganglia fail to properly suppress unwanted movements or to properly prime upper motor neuron circuits to initiate motor function
- a disorder leading to abnormally low output of the basal ganglia leads to relatively no inhibition of the thalamocortical projection neurons. This situation leads to an inability to suppress unwanted movements. These disorders are known as hyperkinetic disorders
- physiotherapy:-
- Correct the abnormal posture by positioning or by using splint: to prevent deformity
Stretching of the contracted muscles: to reduce the spasticity
Soft tissue and joint mobilization: to maintain the joint mobility
Improve muscle tone
Equilibrium exercise :
standing with normal base of support
– standing with eye open / closed
– turning
– sit to stand- Non-Equilibrium exercise: – finger to nose -finger to finger -alternative pronation/supination -tapping of foot -heel to shine
- Parallel bar walking using mirror as a biofeedbackWeight shiftingWalking side wayWalking in uneven surface with support and later progress without using support
Static exercise:- Sit to stand
Stand on both leg with or without support
Stand with eye open and close
Dynamic exercise: Straight walking:-
Tandem walking
Side walking C. Gait training:- Parallel bar walking by placing a mirror in front of the patient will provide
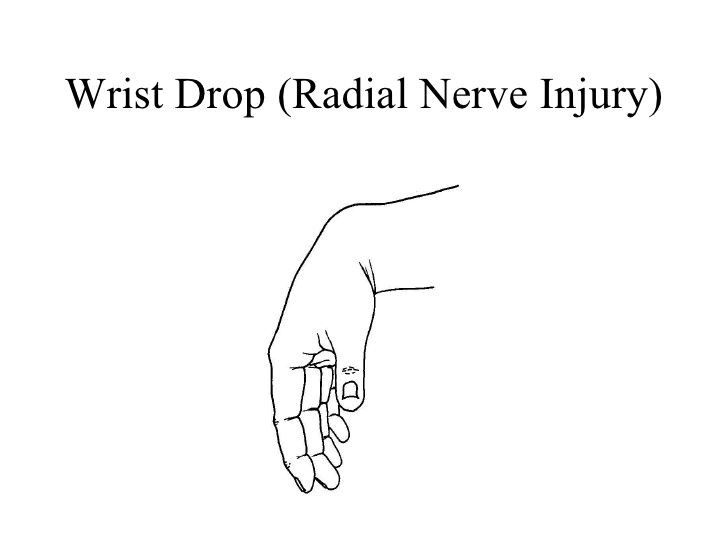
- walk without supportDuring walk promote heel strike at initial contact with the floorPrevent hip dropping and stabilize the pelvis(16) HIGH STEPPIMG GAIT:
- A high steppage gait pattern is one that occurs if you have foot drop
- Foot drop is a condition that is caused by weakness or paralysis of your anterior tibialis muscle
- This muscle contracts to help flex your foot and ankle up while walking.
- This ensures that your foot clears the floor and you do not catch your toes on the ground
- anterior tibialis weakness of paralysis, may exhibit a high steppage gait.
- During this gait pattern, you excessively flex your hip and your knee while you are walking.
- High steppage occurs as you are swinging your leg through the air while stepping forward.
- The hallmark of this gait pattern is that you lift your leg high off the floor, ensuring that you will clear your foot over the ground and not trip.
- Physiotherapy:
- Non-Equilibrium exercise: – finger to nose -finger to finger -alternative pronation/supination -tapping of foot -heel to shine
- Treatment for a high steppage gait pattern involves focusing on the anterior tibialis muscle.
- Specific ankle exercises can help strengthen your anterior tibialis, and stretches for your calf can help ensure that your ankle range of motion (ROM) is well maintained.
- Your physical therapist may choose to use neuromuscular electrical stimulation (NMES) to help improve the way your anterior tibialis muscle works
- This type of electrical stimulation artificially contracts your muscle, helping it to function properly.
- If your anterior tibialis weakness is being caused by sciatica coming from your back, your physical therapist may prescribe back exercises to help get pressure off your sciatic nerve and restore normal function to your leg.
- exercises are designed to allow normal messages to travel up and down your sciatic nerve in your low back.
- Gait training and balance training may also be necessary if you have a high steppage gait
- Your PT may prescribe balance exercises to help improve your overall proprioception.
- You may require an assistive device like a quad cane or a wheeled walker to walk properly.
-Sometimes, paralysis of your anterior tibialis muscle is permanent. If this is the case, you may benefit from a special brace called an ankle-foot orthosis
-This brace helps to lift your foot and toes off the ground. This lessens the likelihood of you stubbing your toes on the ground, and your high steppage gait should go away when you are wearing your AFO. - A temporary solution to anterior tibialis weakness is to use an elastic band to help elevate your foot while you are walking.
- swinging your leg forward, the elastic band pulls your foot up, and your high steppage gait is no longer needed to clear your toes from the ground.
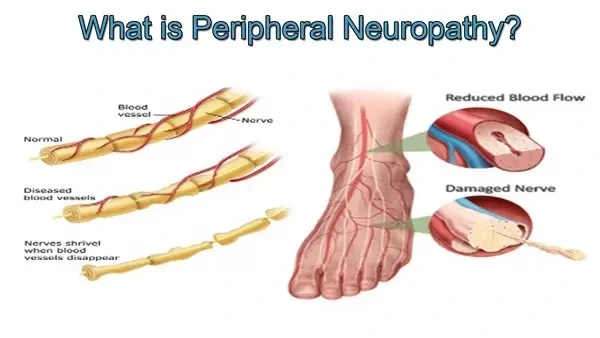
-Seen in patients with foot drop (weakness of foot dorsiflexion), -the cause of this gait is due to an attempt to lift the leg high enough during walking so that the foot does not drag on the floor. -If unilateral, causes include peroneal nerve palsy and L5 radiculopathy. If bilateral, causes include amyotrophic lateral sclerosis, Charcot-Marie
-Tooth disease and other peripheral neuropathies including those associated with uncontrolled diabetes.




Hey! Greetings of the day!
This information proved really helpful in clearing my doubts with respect to gait patterns. Thankyou for sharing.