Shoulder-hand Syndrome (SHS)
Table of Contents
What is a Shoulder-hand Syndrome (SHS)?
Shoulder-Hand Syndrome, also known as Reflex Sympathetic Dystrophy (RSD) or Complex Regional Pain Syndrome (CRPS), is a painful condition that typically affects the upper extremities. It often starts in the shoulder and progresses to the hand, causing stiffness, swelling, and impaired function.
Although the precise etiology of the disease is unknown, injuries or surgeries frequently set it off by causing aberrant nerve responses and inflammation. Early diagnosis and prompt treatment are crucial to prevent the worsening of symptoms and restore mobility.
Types of Shoulder-hand Syndrome (SHS)
There are two kinds of CRPS:
- Type 1 does not entail a direct nerve injury and usually develops as a result of an illness or another accident.
- Type 2 follows a specific nerve damage.
Despite the differences in causes, both kinds of CRPS have the same symptoms and three stages of disease.
Stage I: Acute
Stage I could last no more than 3 months.
Increased sensitivity to touch and scorching pain are the most typical early signs of CRPS. This type of pain is different from what one may anticipate from a particular injury since it is more persistent and constant.
Swelling and joint stiffness are generally followed by increasing warmth and redness in the affected limb.
There may be rapid nail and hair growth and increased sweating.
Stage II: Dystrophic
Stage II might last three to twelve months.
Swelling is more consistent, and skin creases decrease.
Skin temperature drops.
Fingernails get brittle.
Pain is more widespread.
Stiffness increases.
The region that was injured becomes more touch-sensitive.
Stage III: Atrophic
Stage III happens after a year.
The skin in the affected area becomes pale, dry, tight, and glossy.
The area is inflexible, therefore there is little likelihood of recovering movement.
Pain may lessen.
There’s a chance that additional bodily parts will be affected.
Causes of Shoulder-hand Syndrome (SHS)
The cause is yet unknown, but it could be related to one or numerous causes, including.
- Prolonged immobility.
- Minor trauma caused by blood draws and intravenous injections occurred repeatedly.
- Angio-spasm
- Perception deficiency
- Central sympathetic dysregulation and neurogenic inflammatory responses
There are two types of CRPS, and although they have different causes, their symptoms are similar:
- Type 1. This kind, which is sometimes referred to as reflex sympathetic dystrophy, (RSD), appears after a disease or trauma that does not cause the nerves in the affected limb to die outright. Type 1 affects around 90% of CRPS sufferers.
- Type 2. The symptoms of this kind, formerly called causalgia, are the same as those of type one. Sort 2 CRPS, on the other hand, results from a specific sort of nerve injury.
The main cause of many CRPS patients is a major injury to the arm or leg. This could be a crushing wound or a fracture.
Other big and minor traumas, including surgery, heart attacks, infections, and even sprained ankles, can result in CRPS.
Why these experiences can result in CRPS is unknown. Not everyone who has such an accident develops CRPS. It could be the result of an unusual interaction between your central and peripheral neural systems, as well as various inflammatory reactions.
Symptoms and Sign
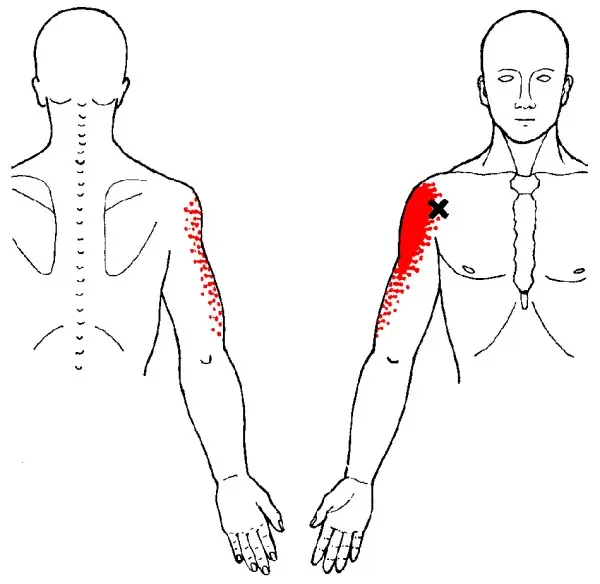
- Shoulder: Loss of range of motion in the shoulder, causing pain and tenderness when moving or resting. Usually, there are no symptoms.
- Wrist: ache during extension, tenderness upon deep palpation, and dorsal edema over carpal bones.
- Hand: little soreness or tenderness, with edema overlaying the metacarpals.
- Digits: The patient may have alterations in hair and nail growth, vasomotor changes, temperature, color, and hidrosis, as well as minor edema and soreness in the metacarpal-phalangeal and interphalangeal joints.
The signs and symptoms of CRPS are:
- Prolonged burning or aching pain, usually in the hand, foot, arm, or leg.
- Sensitivity to touch or cold.
- Swelling around the painful area
- Skin temperature fluctuations—sweating and cold
- Skin tone variations might be red or blue, or blotchy and white.
- Skin texture changes, which might become sensitive, thin, or glossy in the affected area.
- Changes in nail and hair growth
- Joint stiffness, edema, and injury.
- Muscle spasms, tremors, and weakness (atrophy).
Symptoms might change over time and between individuals. Among the initial symptoms include discomfort, edema, redness, temperature fluctuations, and hypersensitivity (especially to touch and cold).
It may have skin and nail alterations, as well as muscular spasms and tightening. The disease is typically incurable at the time these changes take place.
CRPS can occasionally spread from its original location to another part of the body, such as the opposite limb.
Some people’s CRPS symptoms resolve on their own. Others’ indications and symptoms may last for months or years. Treatment is more likely to be beneficial when initiated early in the illness’s progression.
Symptoms of Shoulder-hand Syndrome (SHS)
Pain
- Pain in one or more extremities might be acute, persistent, searing, or deep-aching.
- All tactile contact with the skin (for example, wearing garments or a light breeze) may be interpreted as painful (allodynia).
- Lancinating aches and paroxysmal dysesthesias.
Skin changes
- Skin alterations can include a glossy (dystrophy-atrophy), dry, or scaly appearance.
- Hair may initially become coarse and then thin. The affected extremity’s nails may grow more quickly, become more brittle, and then slow down.
- Rashes, ulcers, and pustules.
- Abnormal sympathetic (vasomotor) activity may be related to skin that feels warm or chilly to the touch.
- Greater sweating (sudomotor alterations) or greater skin cooling caused by goose flesh.
Swelling
- Localized, initially pitting, and then Brawny.
- Edema can be visible.
Movement disorder
- Dystonia may occur.
- Tremors and involuntary jerks of the extremities may occur.
- Disuse causes atrophy in natural history.
Spreading symptoms
- A “continuity type” of spread occurs when symptoms extend upward from the site of origin, for example, from the hand to the shoulder.
- An “independent type” in which symptoms move to a different, distant part of the body. This kind of dissemination might occur naturally or as a result of something else.
- Total body RSD.
Pathology
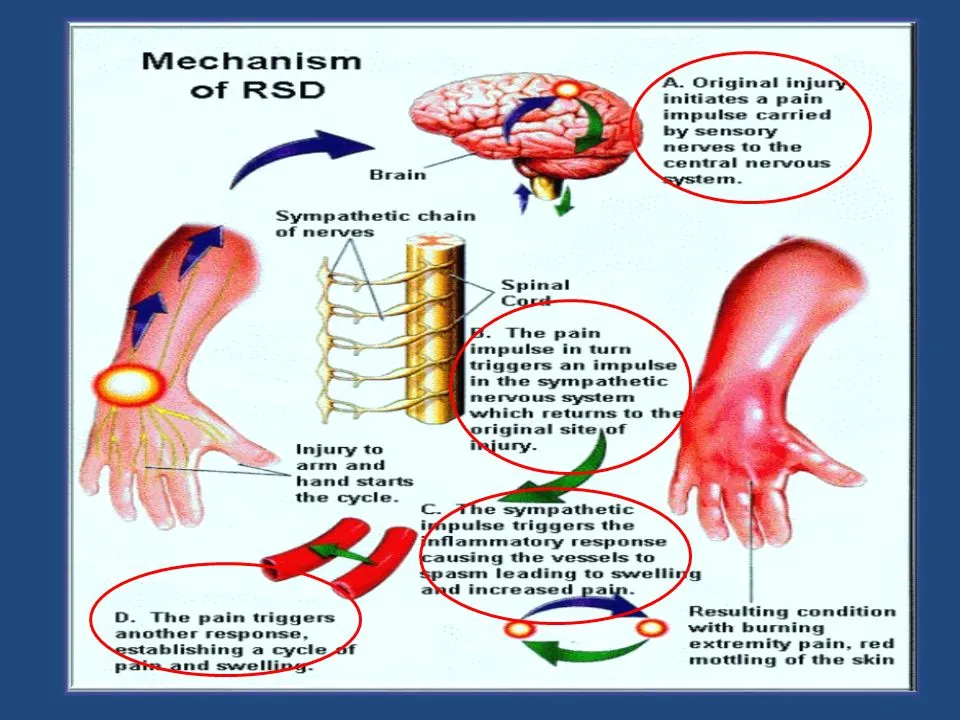
- Sympathetic pain is produced by tonic activity in myelinated mechanoreceptor afferents. Tonic firing in neurons within a nociceptive pathway is triggered by input.
- Damage to central or peripheral brain tissue.
- Patients with polyneuropathy with allodynia had high levels of soluble tumor necrosis factor receptor 1 (sTNF-R1) and increased tumor necrosis factor-alpha activity.
- Pain, vasomotor instability, edema, osteopenia, and cutaneous hypersensitivity associated with shoulder hand syndrome may be caused by distal degeneration of small-diameter peripheral axons.
- Cortical alterations point to a possible pathogenic involvement.
Complications
If CRPS is not identified and treated promptly, more severe symptoms may develop.
- Tissue wasting (atrophy): If you avoid or struggle to move an arm or leg due to pain or stiffness, the skin, bones, and muscles may degenerate and weaken.
- Muscle tightening (contraction): You may also notice muscle tightness. This may cause the hand and fingers, or the foot and toes, to compress into a permanent position.
Diagnosis
One test cannot provide a conclusive diagnosis of CRPS. Nonetheless, the subsequent protocols might offer significant hints:
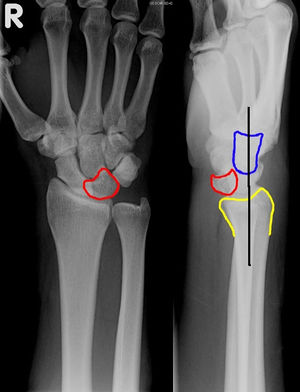
- Bone scan: This technique could help find anomalies in the bones. Once a radioactive material is put into one of your veins, a specialized camera may observe your bones.
- Sweat production testing: Some tests can determine the amount of sweat on both limbs. Uneven results could indicate CRPS.
- X-rays: In the late stages of the disease, mineral loss from your bones may be visible on an X-ray.
- Magnetic resonance imaging, or MRI: Images obtained through a magnetic resonance imaging (MRI) test may reveal tissue alterations that rule out other illnesses.
Treatment of Shoulder-hand Syndrome (SHS)
Nonsurgical Treatment
Prompt diagnosis and treatment are essential to stop CRPS from progressing to more advanced symptoms.
CRPS is a physiological condition (meaning it affects how the body functions, not a person’s emotional or mental state). Even though it is not fully understood, CRPS is managed.
Medications
Physicians treat the symptoms of CRPS with a range of medications.
- Pain remedies: Pain medicines accessible without a prescription, such as aspirin, ibuprofen (Advil, Motrin IB, and others), and naproxen sodium (Aleve), can help with mild pain and inflammation.
- If OTC pain relievers are ineffective for you, your physician may recommend more potent drugs.
- Opioid medicines may be a possibility. When used in small dosages, they may help control pain.
- Antidepressants and anticonvulsants: Sometimes pain from a damaged nerve is relieved by antidepressants like amitriptyline and anticonvulsants like gabapentin (Gralise, Neurontin).
- Corticosteroids: Steroid drugs, such as prednisone, can reduce inflammation and increase mobility in the affected limb.
- Bone loss medicines: Your physician may recommend medications like calcitonin (Miacalcin) and alendronate (Binosto, Fosamax) to stop or slow down the loss of bone.
- Ketamine is administered intravenously: Low intravenous ketamine doses are a powerful anesthetic that can dramatically relieve pain, according to certain studies.
Injection treatment
Pain can be reduced by injecting an anesthetic (numbing medication) close to the sympathetic nerves. This is usually advised early in the course of CRPS to stop the condition from progressing to later phases.
Biofeedback
Pain management may be aided by relaxation methods and an increased awareness of one’s body.
Physical Therapy of Shoulder-hand Syndrome (SHS)
Active exercise focusing on the affected limb’s normal use is critical for long-term relief from this illness. Physical and/or occupational therapy can help patients reestablish normal use patterns. Medications and other treatment options can alleviate pain and allow the patient to participate in active exercise.
- Mirror Therapy: It improves sensory-motor function while also lowering pain and edema in the upper limb in post-stroke patients. This type of therapy uses a mirror to mislead the patient’s brain. Seated in front of a mirror or mirror box, move the leg that is not affected by CRPS so that the brain identifies it as the affected limb. According to research, this form of therapy may assist CRPS patients in enhancing their function and minimizing their pain.
- Orthoses: In stroke survivors, a functional shoulder orthosis helps avoid shoulder subluxation and reduces the prevalence of shoulder-hand syndrome.
- Acupuncture: When combined with a rehabilitation program, acupuncture reduces pain, improves upper limb function, and increases daily activity compared to a rehabilitation program alone. The insertion of long, thin needles may stimulate nerves, muscles, and connective tissue, increasing blood flow and relieving pain.
- Passive and Active R.O.M.: Maintain R.O.M. and shoulder/hand function and reduce pain and edema in the hands.
- LASER therapy is effective for alleviating pain and edema in the affected hand and shoulder, enhancing R.O.M., and boosting independence in post-stroke patients.
- T.E.N.S.: Electrical impulses applied to nerve terminals have the potential to alleviate persistent pain. aids in promoting R.O.M. and reducing pain in the affected shoulder and hand.
- Heat therapy: Putting heat on cold skin might help with pain and edema reduction.
- Spinal cord stimulation: Your physician inserts tiny electrodes into your spinal cord. Pain is reduced when a modest electrical current is applied to the spinal cord.
- Intrathecal medication pumps: This therapy involves pumping pain-relieving medicines into the spinal cord fluid.
Periodically, factors like exposure to cold or severe emotional stress can cause CRPS to recur. Recurrences can be treated with small doses of an antidepressant or another medication.
Surgical Treatment
If nonsurgical treatment fails, surgical techniques may help alleviate symptoms.
- A spinal cord stimulator: Tiny electrodes are inserted along your spine, sending moderate electric impulses to the affected nerves.
- Pain pump implantation: An insignificant abdominal implant supplies the spinal cord with an analgesic.
- The outcomes of surgical procedures might not be as expected: Psychological testing and treatment are beneficial for many individuals with persistent CRPS symptoms.
Prevention
These techniques could lessen your risk of getting CRPS.
- Taking vitamin C after a wrist fracture: According to studies, those who take a lot of vitamin C after a wrist fracture are less likely to develop CRPS than those who don’t.
- Early mobilization following a stroke: Some evidence suggests that persons who get out of bed and walk about shortly after a stroke (early mobilization) have a lower risk of developing CRPS.
Summary
Shoulder-hand syndrome(SHS), also known as reflex sympathetic dystrophy, is a painful condition that affects the shoulder, arm, and hand. Severe pain, stiffness, and swelling in the affected limb are its hallmarks. The exact cause of shoulder-hand syndrome is not fully understood, but it is believed to be related to a malfunction of the sympathetic nervous system.
Shoulder-hand syndrome symptoms usually appear gradually, beginning with shoulder discomfort and stiffness that radiates to the arm and hand. The affected limb may also become swollen and hypersensitive to touch.
Treatment typically involves a combination of pain medication, physical therapy, and sympathetic nerve blocks. If left untreated, the illness may in certain situations result in lifelong impairment. Early diagnosis and treatment are important for improving outcomes for patients with shoulder-hand syndrome.
FAQs
What is shoulder-hand syndrome?
Shoulder-hand syndrome, also known as reflex sympathetic dystrophy, is a chronic pain condition that affects the shoulder, arm, and hand.
Can shoulder-hand syndrome be prevented?
While there is no known way to prevent shoulder-hand syndrome, prompt treatment of any injury or trauma to the shoulder, arm, or hand may help reduce the risk of developing the condition.
References
- Complex Regional Pain Syndrome (Reflex Sympathetic Dystrophy) – OrthoInfo – AAOS. (n.d.). https://orthoinfo.aaos.org/en/diseases–conditions/complex-regional-pain-syndrome-reflex-sympathetic-dystrophy/
- Complex regional pain syndrome – Symptoms & causes – Mayo Clinic. (2022, May 10). Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/crps-complex-regional-pain-syndrome/symptoms-causes/syc-20371151
- Physiotherapist, N. P. (2023, December 13). Shoulder Hand Syndrome Cause, Symptoms, Treatment. Mobile Physiotherapy Clinic. https://mobilephysiotherapyclinic.in/shoulder-hand-syndrome-physiotherapy-management/