Restless Legs Syndrome
Table of Contents
What is The Restless Legs Syndrome?
Restless Legs Syndrome (RLS), also known as Willis-Ekbom Disease, is a neurological disorder characterized by an irresistible urge to move one’s legs. This condition typically occurs during periods of rest or inactivity, such as when sitting or lying down, and is often accompanied by uncomfortable sensations in the legs. Individuals with RLS may describe these sensations as crawling, tingling, itching, or creeping, leading them to constantly move their legs to find relief.
The symptoms of RLS tend to worsen in the evening or at night, which can significantly disrupt sleep and lead to daytime fatigue and sleep disturbances. The exact cause of RLS remains unclear, although genetic factors and abnormalities in dopamine levels in the brain are believed to play a role in its development.
RLS can affect people of all ages, but it is more common in middle-aged and older individuals. It can also occur in pregnant women, where it is referred to as “pregnancy-related RLS.” While RLS is generally a non-life-threatening condition, its impact on quality of life and sleep can be significant, leading to physical and emotional distress.
Simple self-care steps and lifestyle changes might assist relieve symptoms. Medications also assist many more people with Restless Legs Syndrome (RLS).
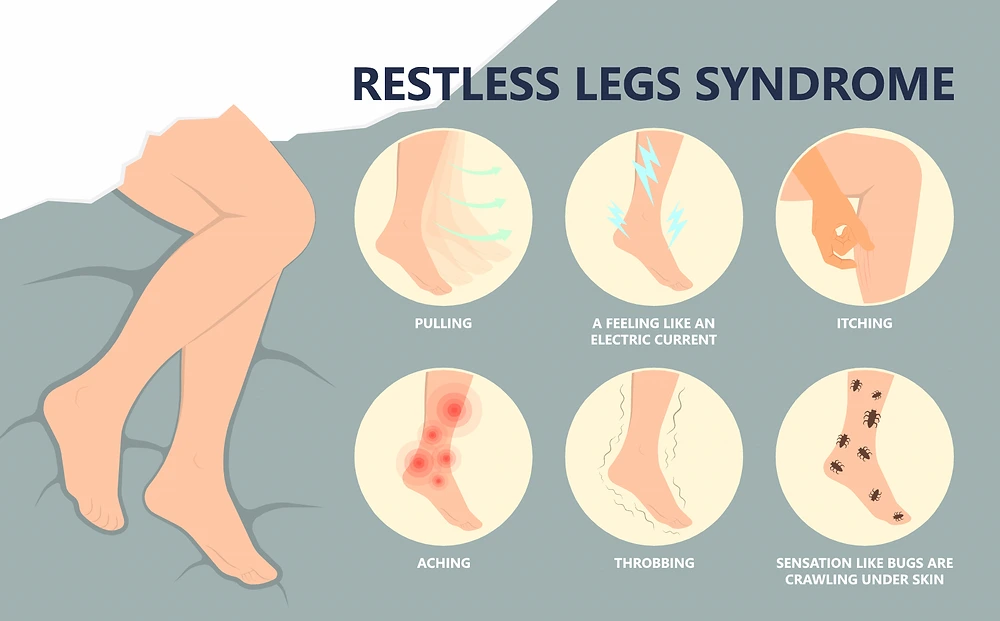
What are the Symptoms of the Restless Legs Syndrome (RLS)?
The chief symptom is a compulsion to move the legs. Common accompanying characteristics of Restless Legs Syndrome (RLS) involve:
- Sensations that begin while resting: The feeling usually starts after you have been lying down or sitting for a while, like in a car, an airplane, or a theatre.
- Relief with movement: The sensation of Restless Legs Syndrome decreases with movement, like the legs jiggling, stretching, or walking.
- Worsening of symptoms in the evening: Symptoms happen mainly at night.
- Nighttime leg twitching: Restless Legs Syndrome (RLS) might be associated with another, much more usual situation called periodic limb movement of sleep, which causes the legs to twitch and kick, maybe throughout the night, while you sleep.
People usually describe Restless Legs Syndrome (RLS) symptoms as compelling, unpleasant sensations in the legs or feet. They normally occur on both sides of the body. A few commonly, the sensations affect the arms.
The sensations, which usually happen within the limb rather than on the skin, are described as:
- Crawling,
- Creeping,
- Pulling,
- Throbbing,
- Aching,
- Itching,
- Electric.
Sometimes the sensations are tough to explain. People with Restless Legs Syndrome (RLS) normally don’t describe the condition as a muscle cramp or numbness. They do, until, frequently describe the desire to move their legs.
It’s usual for symptoms to fluctuate in severity. Sometimes, symptoms depart for periods of time, then come back.
What are the Causes of the Restless Legs Syndrome (RLS)?
Often, there’s no known cause for Restless Legs Syndrome (RLS). Researchers suspect the situation might be caused by a disparity of the brain chemical dopamine, which transmits messages to control muscle movement.
Heredity
Sometimes Restless Legs Syndrome (RLS) runs in families, especially if the condition begins before age 35 to 40. Investigators have recognized sites on the chromosomes where genes for Restless Legs Syndrome (RLS) might be present.
Pregnancy
Pregnancy or hormonal changes might temporarily worsen Restless Legs Syndrome (RLS) signs and symptoms. A few women get Restless Legs Syndrome (RLS) for the first time during pregnancy, especially during his/her last trimester. Until symptoms normally depart after delivery.
Risk factors
Restless Legs Syndrome (RLS) can develop at any age, even during childhood. The condition is much more usual with improving age and is more usual in women than in men.
Restless Legs Syndrome (RLS) normally isn’t related to a crucial underlying medical problem. Until, it sometimes accompanies more conditions, like:
- Peripheral neuropathy: This injury to the nerves in the hands and feet is sometimes due to chronic diseases like diabetes and alcoholism.
- Iron insufficiency: Even without anemia, iron insufficiency can cause or worsen Restless Legs Syndrome (RLS). If you have a history of bleeding from your bowels, experience heavy menstrual periods, or repeatedly donate blood, you might have iron insufficiency.
- Kidney failure: If you have kidney failure, you might also have iron insufficiency, often with anemia. When kidneys don’t function properly, iron stores in the blood can reduce. This and more changes in body chemistry might cause or worsen Restless Legs Syndrome (RLS).
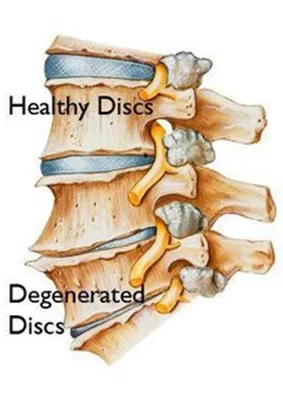
- Spinal cord conditions: Lesions on the spinal cord as a result of injury have been linked to Restless Legs Syndrome (RLS). Having had anesthesia to the spinal cord, like a spinal block, also improves the risk of developing Restless Legs Syndrome (RLS).
- Parkinson’s disease: People who have Parkinson’s disease and take definite drugs called dopaminergic agonists have an improved risk of developing Restless Legs Syndrome (RLS).
Diagnosis
Your doctor provider will take your medical history and ask for a description of your symptoms. A diagnosis of Restless legs syndrome (RLS) depends on the following criteria, established by the International Restless Legs Syndrome (RLS) Study Group:
- You have a strong, often seductive urge to move the legs, commonly accompanied by uncomfortable sensations,
- Your symptoms begin or get worse when you’re resting, like sitting or lying down,
- Your symptoms are temporarily or partially relieved by activity, like walking or stretching,
- Your symptoms are worse at night,
- Symptoms can’t be described solely by another medical or behavioral condition.
Your doctor might conduct physical and neurological tests. Blood tests, particularly for iron deficiency, might be ordered to rule out more possible causes of your symptoms.
In addition, your provider might refer you to a sleep specialist. This might include an overnight stay and a study at a sleep clinic if another sleep disorder like sleep apnea is suspected. Still, A diagnosis of Restless legs syndrome (RLS) normally doesn’t need a sleep study.
Treatment of Restless Legs Syndrome
Although there is no cure for RLS, there are various treatment options available to manage the symptoms and improve the overall well-being of affected individuals. Medical intervention, lifestyle changes, and avoiding certain triggers can all contribute to alleviating the discomfort associated with Restless Legs Syndrome. Consultation with a healthcare professional is essential for an accurate diagnosis and tailored treatment plan for individuals experiencing RLS symptoms.
Sometimes, treating a primary condition, like iron insufficiency, considerably relieves symptoms of Restless Legs Syndrome (RLS). Correcting an iron insufficiency might include receiving iron supplementation orally or intravenously. Still, take iron supplements only with medical management and after your healthcare provider has checked your blood iron level.
If you have Restless legs syndrome (RLS) without an accessory condition, treatment focuses on lifestyle changes. If those aren’t effective, your healthcare provider might advise medications.
Medications
Several prescription drugs, most of which were developed to treat more diseases, are available to decrease anxiety in the legs. These involve:
- Medications that improve dopamine in the brain: These medicines affect levels of the chemical messenger dopamine in the brain. Pramipexole (Mirapex) and Rotigotine (Neupro) are accepted by the Food and Medication Administration for the treatment of moderate to acute Restless legs syndrome (RLS).
- Short-period side effects of these medications are normally mild and involve nausea, lightheadedness, and fatigue. Still, they can also cause impulse control disorders, like compulsive gambling, and daytime sleepiness.
- Drugs affecting calcium channels: Definite medications, like gabapentin (Neurontin, Gralise), gabapentin enacarbil (Horizant), and pregabalin (Lyrica), work for a few people with Restless Legs syndrome (RLS).
- Muscle relaxants and sleep drugs: These drugs assist you to sleep well at night, but they do not detach leg sensations, and they might cause daytime drowsiness. These drugs are commonly only utilized if no more treatment provides relief.
- Opioids: Narcotic medications are utilized mainly to relieve acute symptoms, but they might be addicting if utilized in high doses. A few examples involve codeine, oxycodone (Oxycontin, tramadol (Ultram, ConZip), Roxicodone, and more), and hydrocodone (Hysingla ER).
It might take several trials for you and your healthcare provider to find the right medication or combination of drugs that work best for you.
Caution about medications
Sometimes dopamine drugs that have to perform for a while to relieve your Restless legs syndrome become ineffective, or you notice your symptoms returning earlier in the day or including your arms. This is called augmentation. Your healthcare provider might substitute another medication to combat the problem.
Most medicines prescribed to treat Restless legs syndrome (RLS) aren’t suggested during pregnancy. Instead, your healthcare provider might be suggested self-care methods to relieve symptoms. Still, if the sensations are particularly bothersome during your last trimester, your healthcare provider might approve the utilization of definite medicines.
A few drugs might worsen symptoms of Restless legs syndrome (RLS). These include a few antidepressants, a few antipsychotics, a few nausea-relieving meds, and a few cold and allergy remedies. Your healthcare provider might suggest that you avoid these medicines, if possible. Still, if you require to take these medications, talk to your healthcare provider about adding medicines to assist manage your Restless legs syndrome (RLS).
Physiotherapy Treatment
Yoga and Pilates
Many more professionals suggested yoga, Pilates, and aerobics assist with Restless Legs Syndrome (RLS) symptoms, but they also suggested against almost types of yoga like Ashtanga, hot yoga, or any yoga pose that is especially problematic or that stresses your body.
Cycling
Cycling is another activity that can calm symptoms. To cycle at a moderate pace, target 8 to 10 miles per hour or slightly slower.
Swimming
Swimming or doing water aerobics in a warm pool assists relax your muscles while building strength and increasing mobility.
Stretching Routine
Simple stretching might assist stop Restless Legs Syndrome (RLS) symptoms in their tracks. Here are some stretches to assist you get started.
Calf stretch
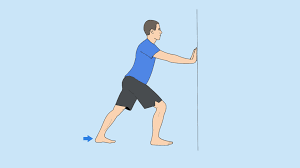
- Stretch out your arms so that your palms are flat opposite a wall and your elbows are nearly straight.
- A small degree bends your right knee and steps your left leg back a foot or two, positioning your heel and foot flat on the floor. Hold for 15 to 30 seconds.
- Next, bend your left knee while holding your heel and foot flat on the floor. For a profound stretch, move your foot back a bit afar.
- Change legs and repeat.
Front thigh stretch
- Standing collateral to a wall for balance, pull one of your ankles about your rear while keeping the other leg straight.
- Hold for 15 to 30 seconds.
- Change legs and repeat.
Hip flexor stretch
- Place the back of a chair opposite the wall for help and stand facing the chair.
- Improve your left foot up and relax it flat on the chair, with your knee bent. (Or try placing your foot on a stair while keeping the railing for balance.)
- Press your pelvis forward gently until you feel a stretch at the top of your right thigh while keeping your spine as neutral as possible. Your pelvis will move ahead only a little.
- Hold for 15 to 30 seconds.
- Change legs and repeat.
Gentle to moderate exercise can assist with your Restless Legs Syndrome (RLS) symptoms. Talk to your doctor about effective weekly day-to-day that will work best for you. If you are pregnant, be sure to check with them about safe activities for you.
Lifestyle and home remedies
Making simple lifestyle changes can assist alleviate symptoms of Restless legs syndrome (RLS):
- Try baths and massages: Soaking in a warm bath and massaging the legs can release the muscles.
- Apply warm or cool packs: Utilize cold or heat, or alternating use of the two, which might decrease the limb sensations.
- Begin good sleep hygiene: Tiredness tends to aggravate symptoms of Restless legs syndrome (RLS), so it is main that you practice good sleep hygiene. Ideally, have a cool, quiet, and well-sleeping environment go to bed and improve at a similar time daily; and get at least 7 (seven) hours of sleep nightly.
- Exercise: Getting moderate, routine exercise might relieve symptoms of Restless legs syndrome (RLS), but overworking it or working out too late in the day might intensify symptoms.
- Avoid caffeine: Sometimes cutting back on caffeine may assist restless legs. Avoid caffeine-containing products, including chocolate, coffee, tea, and soft drinks, for a few weeks to see if this assists.
- Consider using a foot wrap or a vibrating pad: Pressure is applied to the foot when wearing a foot wrap, which may help with symptoms of restless legs syndrome. You might also find relief utilize a pad that vibrates on the back of the legs.
Coping and support
Restless legs syndrome (RLS) is commonly a lifelong condition. It might assist you to develop coping strategies that work for you, like:
- Tell others about your Restless Legs Syndrome (RLS) condition: Sharing information about Restless Legs syndrome (RLS) will assist your friends, family members, and co-workers in good understanding when They observe you while you walk to the water cooler, pace the hallways or stand in the back occasionally.
- Do not withstand your requirement for movement: If you target to suppress the urge to move, you might detect that your symptoms worsen.
- Keep a sleep diary: Hold track of the strategies and drugs that support your battle with Restless Legs Syndrome, and share this information with your doctor.
- Stretch and massage: Begin and finish your day with stretching exercises and gentle massage.
- Seek help: Support groups bring together family members and people with Restless legs syndrome (RLS). Your insights can help you and possibly someone else by taking part in a group.
Key points about Restless Legs Syndrome (RLS)
- Restless Legs Syndrome (RLS) is a disorder that causes dislike sensations in the legs. The cause of Restless Legs Syndrome (RLS) is still unknown.
- With Restless Legs Syndrome (RLS), you have a seductive compulsion to move the affected limb when the sensations happen.
- Your doctor can diagnose Restless Legs Syndrome depending on your health history, your symptoms, and your physical exam, but there is no definitive exam to diagnose Restless Legs Syndrome (RLS).
- Lifestyle and drug changes can assist ease Restless Legs Syndrome (RLS) symptoms.
Next steps
Tips to assist you get the most from a visit to your medical officer provider:
- Know the cause of your visit and what you want to occur.
- Before your visit, write down the questions you want to respond to.
- Bring someone with you to assist you ask questions and remember what your doctor provider tells you.
- Take note of any new diagnoses, medications, tests, or treatments during the appointment. Note whatever directions your doctor provides you as well.
- Know why a drug or treatment is advised, and how it will assist you. Too, know what the side effects are.
- Ask if your situation can be treated in more ways.
- Know why an exam or procedure is suggested and what the outcomes could mean.
- Know what to expect if you do not take the drug or have the exam or procedure.
- If you have a follow-up appointment, write down the time & date, and intention for that visit.
- Know how you can contact your doctor provider if you have questions.
What you can do in the meantime?
To ease your symptoms, try:
- Cutting back on or eliminating tobacco, caffeine, and alcohol
- Massaging your both legs while soaking in a warm bath
FAQs
In most patients, the cause of Restless Legs Syndrome (RLS) is unknown. However, Restless Legs Syndrome (RLS) often runs in families and special gene variants have been associated with the situation. Low levels of iron in the brain also might be answerable for Restless Legs Syndrome (RLS). Restless Legs Syndrome also might be related to a dysfunction in an area of your brain that controls movement.
Use of heat or cold packs, or alternating use of the two, might lessen the limb sensations. Begin well sleep hygiene. Fatigue tends to worsen symptoms of Restless Legs Syndrome (RLS), so it is main that you practice good sleep hygiene.
Taking vitamin B6 and magnesium supplements can decrease the severity of symptoms of Restless Legs Syndrome (RLS) patients and increase their sleep quality.
Day-to-Day activity, involving lower-body resistance training And aerobic exercise, can obviously decrease the symptoms of Restless Legs Syndrome in most people. Choose the exercises you enjoy, especially those that emphasize utilizing the legs.
Eat a protein snack before bedtime, like a hard-boiled egg, a bit of chicken, or meat to keep your blood sugar stable. Low blood sugar is a trigger for Restless Legs Syndrome (RLS), and protein stabilizes. Avoid sweets or carbohydrates before bedtime, which causes a spike and then a crash in blood sugar.
Abstract. Restless Legs Syndrome is a neurological sleep confusion with frequent (40%) coexisting psychiatric comorbidities. Patients with any psychiatric comorbidity had some periodic leg movements in sleep. Psychiatric disorders should be taken into account in patients with Restless Legs Syndrome.
The early-onset form start before the age of 40 to 45, and sometimes as early as childhood. The signs and symptoms of this form normally worsen slowly with time. The late-onset form start after age 45 to 50, and its signs and symptoms tend to worsen other rapidly.
In most cases, the occasion of Restless Legs Syndrome (RLS) is unknown. However, Restless Legs Syndrome (RLS) oft runs in special, and families of gene variants have been associated with the disease. Low levels of iron in the brain also might be responsible for Restless Legs Syndrome (RLS). Restless Legs Syndrome (RLS) also might be related to a dysfunction in an area of your brain that controls movement




3 Comments