Dysphagia
Table of Contents
Definition
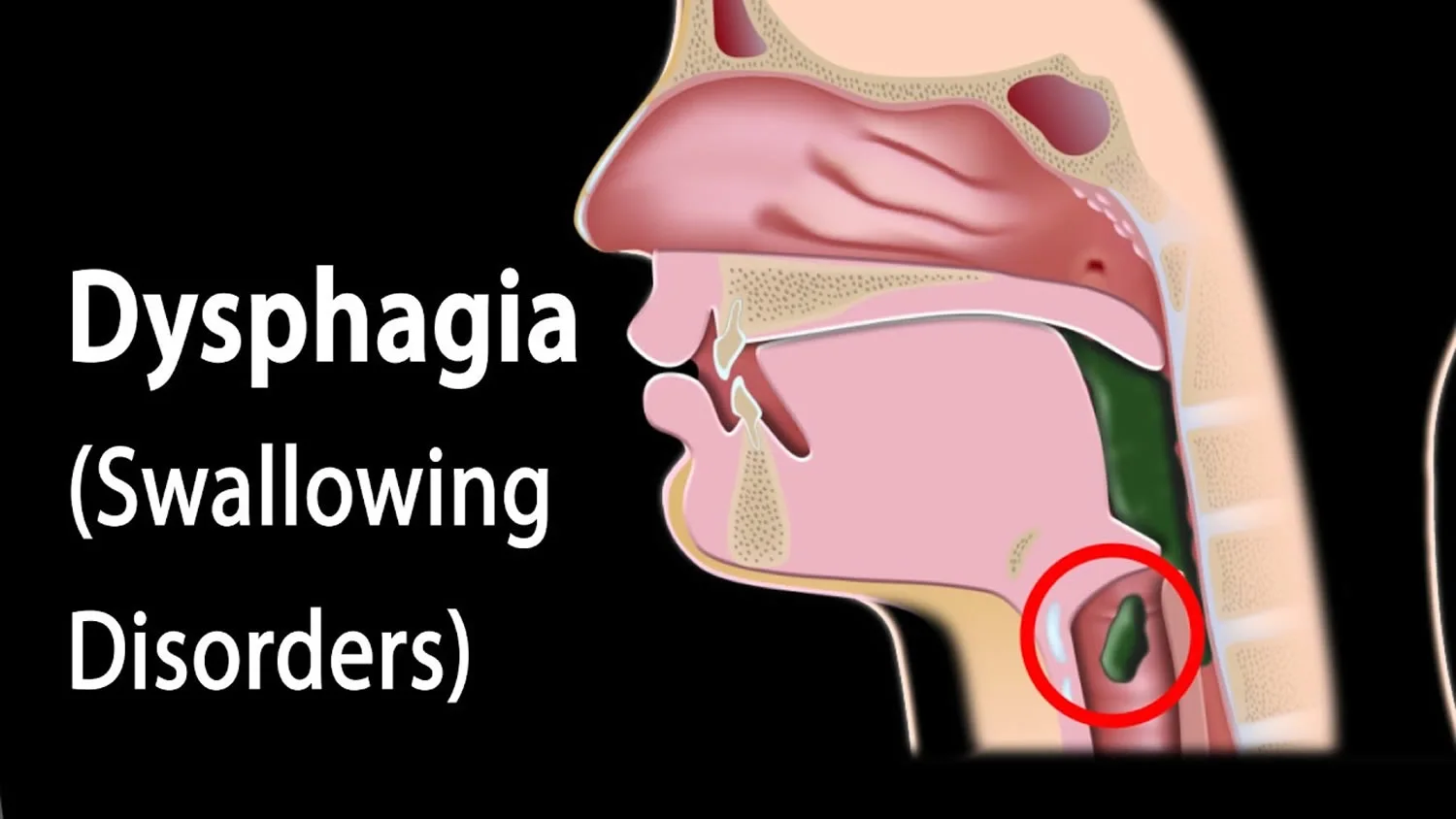
Dysphagia is a medical condition characterized by difficulty swallowing food or liquids. It is a common condition that can affect people of all ages, from infants to the elderly. Dysphagia can be caused by a variety of factors, including neurological disorders, muscular disorders, structural abnormalities, and other medical conditions.
In this article, we will explore the causes, symptoms, diagnosis, and treatment of dysphagia.
Types of Dysphagia
There are two types of dysphagia: oropharyngeal dysphagia and esophageal dysphagia.
- Oropharyngeal dysphagia: This type of dysphagia occurs when there is a problem with the swallowing mechanism in the mouth and throat (pharynx). It is often caused by neurological disorders, such as stroke, Parkinson’s disease, or multiple sclerosis, or muscular disorders, such as myasthenia gravis. Symptoms of oropharyngeal dysphagia include difficulty initiating a swallow, coughing or choking while swallowing, and regurgitation of food or liquid through the nose or mouth.
- Esophageal dysphagia: This type of dysphagia occurs when there is a problem with the esophagus, the tube that carries food from the throat to the stomach. It is often caused by structural abnormalities, such as a narrow esophagus or tumors in the esophagus, or by conditions that affect the muscles or nerves of the esophagus, such as achalasia or scleroderma. Symptoms of esophageal dysphagia include a sensation of food getting stuck in the chest or throat, chest pain, and heartburn.
It is important to identify the type of dysphagia in order to determine the appropriate treatment. Oropharyngeal dysphagia may be treated with exercises to improve swallowing, changes to the texture or consistency of food, or medications to relax the muscles of the throat. Esophageal dysphagia may be treated with medications to reduce inflammation or acid reflux, dilation of the esophagus to widen it, or surgery to correct structural abnormalities.
Causes of Dysphagia
Dysphagia can have a variety of causes, which can be divided into two main categories: neurological causes and structural causes.
Neurological causes:
Dysphagia may be caused by neurological disorders that affect the nerves and muscles involved in swallowing. These can include:
- Stroke: A stroke can damage the part of the brain that controls swallowing.
- Parkinson’s disease: This condition can cause the muscles in the mouth and throat to become weak or rigid, making it difficult to swallow.
- Multiple sclerosis: This condition can damage the nerves that control the muscles involved in swallowing.
- Amyotrophic lateral sclerosis (ALS): This condition can cause weakness and wasting of the muscles involved in swallowing.
Structural causes:
Dysphagia may also be caused by structural abnormalities in the mouth, throat, or esophagus. These can include:
- Esophageal stricture: a narrowing of the esophagus that can be caused by scar tissue, tumors, or acid reflux.
- Gastroesophageal reflux disease (GERD): This condition can cause stomach acid to flow back into the esophagus, irritating and inflaming the lining of the esophagus.
- Tumors: Tumors in the mouth, throat, or esophagus can interfere with swallowing.
- Zenker’s diverticulum: A pouch that forms in the esophagus and can trap food, making swallowing difficult.
- Cervical spine abnormalities: Abnormalities in the bones of the neck can compress the esophagus and make swallowing difficult.
Other factors that can contribute to dysphagia include aging, certain medications that can dry out the mouth or affect muscle function, and radiation therapy to the head and neck.
Symptoms
The main symptom of dysphagia is difficulty swallowing food or liquid. This can manifest in different ways depending on the type of dysphagia and its underlying cause. Here are a few most common symptoms of dysphagia:
Oropharyngeal dysphagia:
- Difficulty initiating a swallow
- Coughing or choking while swallowing
- Regurgitation of food or liquid through the nose or mouth
- Nasal congestion or voice changes after swallowing
- Frequent pneumonia or respiratory infections due to food or liquid entering the lungs
Esophageal dysphagia:
- A sensation of food sticking in the chest or throat
- Chest pain or discomfort during or after swallowing
- Heartburn or acid reflux
- Difficulty swallowing pills or solid foods, but not liquids
- Regurgitation of food or sour liquid
In severe cases of dysphagia, there may be unintended weight loss due to difficulty eating or drinking enough. Dysphagia can also cause anxiety and social isolation, as people may avoid eating or drinking in public due to embarrassment or fear of choking.
Diagnosis
The diagnosis of dysphagia involves a combination of medical history, physical examination, and tests to evaluate the swallowing mechanism and identify the underlying cause. Here are some common diagnostic methods for dysphagia:
- Medical history: The doctor will ask questions about the patient’s symptoms, including when they started, what triggers them, and whether there are any associated conditions such as acid reflux or neurological disorders.
- Physical examination: The doctor will examine the mouth, throat, and neck for signs of structural abnormalities or muscle weakness. They may also check for signs of aspiration (food or liquid entering the lungs) such as coughing, wheezing, or crackling sounds.
- Swallowing tests: These tests evaluate the function of the swallowing mechanism and can be performed by a speech-language pathologist or a gastroenterologist. They may include:
- Video fluoroscopy: This test involves swallowing a liquid containing barium while X-ray images are taken to visualize the swallowing process.
- Fiberoptic endoscopic evaluation of swallowing (FEES): This test involves inserting a flexible tube with a camera through the nose to view the swallowing process and assess the function of the pharynx and larynx.
- Manometry: This test measures the pressure and coordination of the muscles involved in swallowing.
- Imaging tests: These tests can help identify structural abnormalities such as tumors or strictures. They may include:
- CT scan or MRI: These tests produce detailed images of the mouth, throat, and esophagus.
- Barium swallow: This test involves swallowing a liquid containing barium, which shows up on X-ray images and can help identify blockages or abnormalities.
Once the underlying cause of dysphagia is identified, the doctor can develop a treatment plan tailored to the patient’s specific needs.
Treatment of Dysphagia
The treatment of dysphagia depends on the underlying cause, severity of symptoms, and the individual’s overall health. Here are some common treatments for dysphagia:
- Swallowing therapy: This involves working with a speech-language pathologist who specializes in swallowing disorders. They can teach exercises to strengthen the muscles involved in swallowing and improve coordination. They can also suggest strategies to make swallowing easier, such as adjusting head and body position or modifying the texture of food and liquid.
- Dietary modifications: Certain foods and textures may be easier to swallow than others. A speech-language pathologist or a registered dietitian can recommend a diet that is easier to swallow and provides adequate nutrition. This may include pureed foods, thickened liquids, or foods that are moist and easy to chew.
- Medications: In some cases, medications may be prescribed to treat the underlying condition causing dysphagia, such as acid reflux or neurological disorders.
- Surgery: If dysphagia is caused by a structural abnormality, such as a tumor or strictures, surgery may be necessary to remove the obstruction or widen the esophagus.
- Feeding tubes: In severe cases where swallowing therapy and dietary modifications are not effective, a feeding tube may be necessary to provide nutrition and hydration.
- Lifestyle modifications: Certain lifestyle changes may help reduce symptoms of dysphagia, such as avoiding alcohol and tobacco, maintaining a healthy weight, and practicing good oral hygiene.
It is important to seek medical attention if you experience difficulty swallowing, as untreated dysphagia can lead to serious complications such as malnutrition, dehydration, and pneumonia. A multidisciplinary approach involving a neurologist can help manage dysphagia and improve the quality of life.
Physiotherapy management
Physiotherapy can play an important role in the management of dysphagia by working on improving the strength and coordination of the muscles involved in swallowing. Here are some common physiotherapy techniques used in the management of dysphagia:
- Exercise-based therapy: A speech-language pathologist or physiotherapist can prescribe exercises that focus on improving the strength and coordination of the swallowing muscles. These exercises may include head and neck exercises, tongue and lip exercises, and exercises that target the muscles used in breathing.
- Neuromuscular electrical stimulation (NMES): This technique involves the use of a low-level electrical current to stimulate the swallowing muscles, which can improve muscle strength and coordination.
- Thermal stimulation: This involves the use of cold or hot liquids to stimulate the swallowing reflex and improve muscle coordination.
- Biofeedback: This technique uses sensors to monitor muscle activity during swallowing and provides feedback to the patient to help them improve their swallowing technique.
- Positioning techniques: Certain body positions can make swallowing easier. A physiotherapist can recommend positions that facilitate swallowing, such as tilting the head forward or sideways.
- Education and counseling: A physiotherapist can educate the patient and their family members on ways to modify their diet and eating habits to make swallowing easier. They can also provide counseling on ways to cope with the emotional and social impact of dysphagia.
Overall, physiotherapy can play an important role in the management of dysphagia, working alongside a neurologist to provide a comprehensive treatment plan.
Precaution
Patients with dysphagia should take particular precautions to decrease the risk of choking or aspiration. Here are some precautions that should be followed:
- Eat slowly: Eating slowly and taking smaller bites can help to prevent choking and make swallowing faster and easier.
- Sit upright while eating: Sitting upright can help ensure that food and liquids go down the esophagus and not into the lungs.
- Avoid distractions while eating: Focusing on eating and not talking or watching television can help prevent choking.
- Cut food into small pieces: Chopping food into small pieces can make it easier to swallow.
- Avoid tough, dry, or hard-to-swallow foods: Foods that are tough to chew or swallow, such as raw vegetables or tough meat, should be avoided.
- Modify the texture of food and liquids: Depending on the severity of the dysphagia, the texture of food and liquids may need to be modified, such as by being pureed or thickened.
- Take medications as directed: Medications should be taken as directed by a healthcare professional to prevent side effects that may worsen dysphagia.
- Stay hydrated: Staying hydrated can help prevent a dry mouth and throat, which can make swallowing more difficult.
- Practice good oral hygiene: Maintaining good oral hygiene can prevent infections that may lead to inflammation and swelling of the throat, which can contribute to dysphagia.
By taking these precautions, patients with dysphagia can decrease the risk of complications and promote safer swallowing. It is necessary to consult with a doctor for individualized advice on managing dysphagia.
Conclusion
Dysphagia is a common medical condition that can be caused by a variety of factors, including neurological disorders, structural abnormalities, and other medical conditions. The symptoms of dysphagia can vary depending on the underlying cause but may include difficulty swallowing food or liquid, coughing or choking while eating, and regurgitation of food or liquid. The diagnosis usually involves a physical examination and a variety of tests, such as a swallowing test, an endoscopy, or a barium swallow test. Treatment depends on the underlying cause and may include medication, surgery, or a feeding tube. Prevention involves eating slowly, chewing food thoroughly, avoiding difficult-to-swallow foods, and quitting smoking and alcohol.
FAQs
What are the four stages of dysphagia?
Dysphagia is the medical term for difficulty swallowing. There are typically four stages of dysphagia that can be used to assess the severity of the condition. These stages are:
Oral preparatory stage: This stage involves the preparation of food or liquid in the mouth prior to swallowing. During this stage, the food is chewed and mixed with saliva to form a bolus that is ready to be swallowed.
Oral stage: This stage involves the movement of the bolus from the front of the mouth to the back of the mouth, where the swallowing reflex is triggered. In this stage, the tongue and other muscles in the mouth and throat work together to move the bolus toward the pharynx.
Pharyngeal stage: This stage involves the movement of the bolus through the pharynx and into the esophagus. During this stage, the larynx (voice box) closes to prevent food or liquid from entering the airway, and the muscles in the pharynx contract to push the bolus down into the esophagus.
Esophageal stage: This stage involves the movement of the bolus through the esophagus and into the stomach. In this stage, the muscles in the esophagus contract in a coordinated manner to move the bolus downward toward the stomach.Can dysphagia be cured?
The possibility of a complete cure for dysphagia depends on the underlying cause of the condition. In some cases, such as those caused by a temporary illness or injury, dysphagia may resolve on its own as the underlying condition heals. However, in many cases, dysphagia is a chronic condition that requires ongoing management.
Treatment of dysphagia typically involves a multidisciplinary approach that includes a combination of dietary modifications, swallowing exercises, and sometimes medication or surgical interventions. For example, speech therapists can provide exercises to strengthen the muscles involved in swallowing, while dietitians can recommend modified food textures and consistencies to make swallowing easier.What are the leading causes of dysphagia?
Dysphagia can be caused by a variety of factors, including neurological disorders such as Parkinson’s disease, stroke, multiple sclerosis, and muscular dystrophy. It can also be caused by structural abnormalities, such as a narrow esophagus, or tumors in the throat or esophagus. Other medical conditions that can cause dysphagia include GERD (gastroesophageal reflux disease), scleroderma, and certain medications.
Can you live with dysphagia?
Yes, it is possible to live with dysphagia, but the severity and impact on daily life can vary depending on the individual and the underlying cause. Dysphagia can make it difficult to eat and drink and can lead to malnutrition, dehydration, and other complications if not managed properly.
However, there are various treatment options available that can help manage dysphagia and improve quality of life. For example, dietary modifications such as changing the texture or consistency of food and drink can make swallowing easier. Swallowing exercises provided by a speech therapist can also help to strengthen the muscles involved in swallowing and improve swallowing function.What deficiency causes dysphagia?
There are several vitamin and mineral deficiencies that can potentially cause dysphagia, but it is important to note that dysphagia is usually caused by other underlying medical conditions, rather than nutrient deficiencies.
One possible deficiency that can cause dysphagia is vitamin B12 deficiency, which can lead to neurological problems, including difficulty swallowing. Vitamin B12 deficiency can be caused by a variety of factors, including poor absorption of the vitamin in the digestive system or a lack of dietary intake of vitamin B12.





2 Comments