Deep Tendon Reflex (DTR)
Table of Contents
Introduction
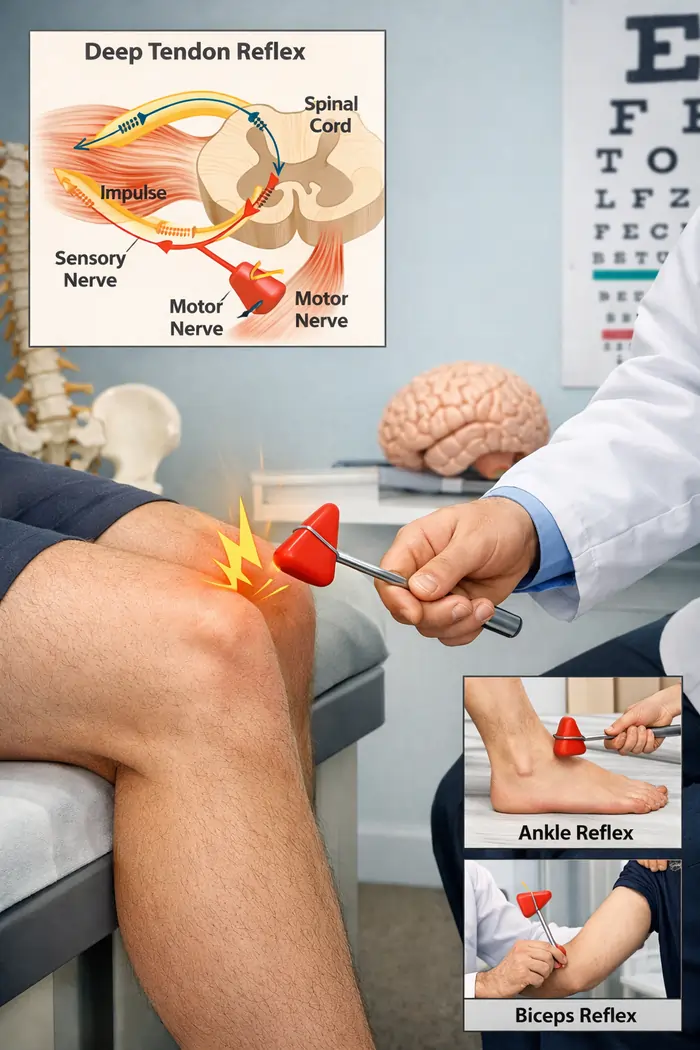
The deep tendon reflex (DTR), initially identified by Wilhelm Heinrich Erb and Carl Friedrich Otto Westphal in 1875, is crucial for assessing and identifying neurologic disorders. Assessing neurologic diseases that impact afferent nerves, spinal cord synaptic connections, motor nerves, and descending motor pathways can be facilitated by deep tendon reflexes, also known as the “muscle stretch reflex.”
The presence of hyporeflexia or hyperreflexia is regarded as a “hard sign” of neurologic dysfunction, and accurate technique and result interpretation are essential for distinguishing between upper and lower motor neuron pathologic processes, including multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), spinal cord injuries, and spinal muscular atrophies.
Major deep tendon reflex
- Muscle involved: biceps brachii
- Nerve supply: musculocutaneous
- Segmental innervation: C5-C6
- Brachioradialis Reflex
- Muscle involved: brachioradialis
- Nerve supply: radial
- Segmental innervation: C5-C6
- Triceps Reflex
- Muscle involved: triceps brachii
- Nerve supply: radial
- Segmental innervation: C7-C8
- Patellar Reflex (knee-jerk)
- Muscle involved: quadriceps femoris
- Nerve supply: femoral
- Segmental innervation: L2-L4
- Achilles Reflex (ankle-jerk)
- Muscles involved: gastrocnemius, soleus
- Nerve supply: tibial
- Segmental innervation: S1-S2
The National Institute of Neurological Disorders and Stroke (NINDS) developed a grading system ranging from 0 to 4 in 1993 to establish a uniform scale for evaluating deep tendon reflexes. This verified scale has been used extensively.
NINDS grades deep tendon reflexes.
- 0: No reflex
- A trace response or a reaction elicited solely by reinforcement is an example of a tiny, below-normal reflex.
- A reflex that occurs within the normal range.
- The top half of a normal range for reflex
- Reflex increased more than usual, including clonus if present, which may be mentioned in another verbal description of the reflex.
Usually, what is considered “normal” is determined by the patient’s history and previous recorded reflex grade. The presence of asymmetric responses suggests abnormality. For comparison, the examiner should try the same response on the other side after obtaining one on the first.
Important Issues
Because of the stretch action and the resulting muscle response, the deep tendon reflex is often referred to as the stretch reflex or myotatic reflex. They are not the same reflex, according to some writers. They think that when the tendon is tapped with a hammer, the tendon reaction happens after the tendon has actively stretched.
The stretch response, on the other hand, happens after the muscle spindle has been continuously stretched during posture and walking. The stretch reflex has a high delay, but the tendon reflex has a quick one.
Mechanism
An involuntary use that triggers a muscular response in a tendon is called a reflex arc. Because there is just one synapse connecting the two neurons—a sensory and a motor neuron—it is referred to as a monosynaptic reflex. The sensory neuron innervates the muscle or the Golgi tendon organ connected to the muscle and supplies the afferent component. It is composed of a cell body located in the dorsal root ganglion (DRG).
The alpha motoneuron in the anterior horn of the spinal cord is part of the motor neuron, which supplies the efferent component. The muscle spindle, a proprioceptive organ, is where the pathway starts. The muscle spindle, which senses muscle stretch, is made up of intrafusal fibers that are covered in a connective tissue capsule. The muscle spindle is located within the muscle, between the extrafusal fibers.
Tendons, muscles, and the reflex arc are all involved in the process of causing a deep tendon reflex in a patient. The related muscle passively stretches when the associated tendon is tapped. The muscle spindle, which is found inside the muscle fibers, senses the strain of the muscle fiber. Made up of intrafusal fibers that do not contract, the muscle spindle is a sensory proprioceptor that decides the length of the muscle fibers.
Action potentials are produced by the muscle spindles’ Ia afferent sensory fibers in response to the strain. The alpha motor neuron that sends signals to the homonymous muscle extrafusal fibers is monosynaptically stimulated by these Ia afferent fibers, which travel to the spinal cord at the dorsal root. The neurotransmitter at the central synapse is glutamate. Then, to oppose this stretch, the extrafusal muscle fibers contract. The reflex is stopped when the muscular contraction takes place because the muscle spindle lowers the action potential firing frequency.
During the reflex, the agonist muscle contracts while the antagonistic muscle is inhibited. Alpha motor neurons to the antagonistic muscle are inhibited by the Ia inhibitory interneuron, causing this action to occur polysynaptically. For instance, the quadriceps muscles contract and are activated during the knee-jerk response, while the hamstring muscles are relaxed and inhibited. The gamma motor neuron in the muscle spindle controls the sensitivity of the muscle spindle and the reflex response by causing intrafusal muscle fibers to tighten or relax. Acetylcholine acts as a bridge in this.
Reflexes of the deep tendons
Biceps reflex
Place the patient’s forearm halfway between flexion and extension on the examiner’s forearm to support it. With fingers curled over the elbow, the examiner should place their thumb firmly over the biceps tendon. Tap quickly. At the elbow, the forearm should flex.
Triceps reflex
Support the patient’s forearm by placing it halfway between flexion and extension on the examiner’s forearm. The olecranon is where the triceps insertion should be found. Just over the insertion, tap. Expanding the forearm is required.
Brachioradialis reflex
Identify the brachioradialis tendon at the wrist while supporting the patient’s arm at the elbow. It inserts near the base of the radius’s styloid process, approximately 1 centimeter laterally from the radial artery. The patient’s biceps tendon should be supported by the thumb of the hand holding their elbow. Using the other hand, tap the brachioradialis tendon. The brachioradialis reflex will cause the forearm to flex and flex. This procedure may also cause the finger jerk reflex, which manifests as flexing of the fingers.
Knee Jerk reflex
The examiner should place one hand on the patient’s quadriceps while the patient’s legs swing freely on the side of the examination table. Check for contraction of the quadriceps and extension of the leg at the knee by tapping the patellar tendon.

Ankle Jerk reflex
The examiner should place one hand beneath the sole of the patient’s foot and dorsiflex it gently as the patient’s legs swing freely on the side of the examination table. Just above where it attaches to the calcaneus, tap the Achilles tendon. In reaction, the foot should plantarflex.
If there isn’t an obvious reaction at first when testing lower extremity reflexes like the patellar or ankle reflex, the examiner may then employ the Jendrassik procedure. The patient performs this motion by flexing their elbows, clenching their teeth, and forcefully interlocking both sets of fingers. The patient is told to keep their hands linked while pulling them apart.
Some of the descending inhibition that the brain sends to the lower motor neuron reflex arc is countered by the voluntary innervation of the top motor neurons caused by this technique. Additionally, because the patient is more focused on the movement and less on the examiner, it keeps them from actively inhibiting the reflex.
Pathophysiology
Lesions in the higher motor neurons cause hyperactive deep tendon reflexes. Pathologically, a superior lesion—a lesion above the level of the spinal reflex pathways—may cause hyperactive DTRs, which could be the first indication of abnormalities in the corticospinal tract or other descending pathways affecting the reflex arc.
A considerably lighter tendon tap than usual may cause hyperactive DTRs, which have a short latency and may exhibit reflex muscular activity in motor neuron pools of synergistic muscles. For instance, wrist pronation may result from a tendon tap to the biceps brachii.
Lower motor neuron lesions are defined by hypoactive or absent deep tendon reflexes. Disease conditions such as beta-blockade, hypothyroidism, hypothermia, and cerebellar dysfunction can cause hypoactive DTRs.A lesion within the reflex arc is indicated by absent DTRs. A lesion impacting the reflex’s afferent arc, either the nerve or the dorsal horn, is indicated by the presence of an absent response and sensory loss in the reflex’s nerve distribution. A lesion involving the efferent arc, anterior horn cells, efferent nerve, or both is indicated by an absence reflex plus paralysis, fasciculations, and muscle atrophy. The most frequent cause of areflexia is peripheral neuropathy, which is usually caused by pollutants, diabetes, alcoholism, uremia, vitamin deficiencies, or amyloidosis.
Although peripheral neuropathy is typically indicated by a bilateral absent ankle jerk, cauda equina syndrome can also provide this result. DTRs may also be absent or reduced as a result of some peripheral nerve lesions. Depending on the anatomical location of the nerve damage, a radial nerve injury may impact the triceps or brachioradialis response, whereas a musculocutaneous nerve injury might affect the biceps reflex. Ankle reflexes can be impacted by tibial nerve lesions, and patellar reflexes by femoral nerve lesions.
Clinical Importance
The DTR gives information on the health of upper and lower motor neurons and is used to evaluate the integrity of the motor system. If a lower motor neuron (nerve roots or peripheral nerves) is injured or diseased, a hypoactive or absent reflex will be observed. If the higher motor neuron (brain, brainstem, or spinal cord) is damaged, there will be a hyperactive reflex.
A lesion in the descending motor neurons can induce clonus, which is the involuntary and rhythmic contraction of muscles, in severe chronic instances that usually come by spasticity. Patients with multiple sclerosis, stroke, spinal cord injury, or cerebral palsy frequently experience clonus. It can also happen after consuming high doses of serotonergic substances. Clonus, if present, is never a normal finding and requires more workup, whereas hyperreflexia, particularly if bilateral, can be a normal finding.
Localizing the lesions can be aided by knowledge of reflex laterality. Assume, for instance, that the right side of the body has normal reflexes but the left side has hyperactive ones. Then, somewhere above the level of the highest hyperactive reaction, it can be deduced that there is a lesion disrupting the corticospinal circuits.
A useful technique to determine how a pregnant patient will react to magnesium infusions is the deep tendon reflexes. Since magnesium sulfate works by inhibiting the central nervous system (CNS), it is the main drug used to prevent and treat eclamptic seizures. New-onset loss of DTRs is one of the earliest indicators of magnesium toxicity and is a clear indication that magnesium infusion needs to be ended right away.