Muscle Stiffness
Table of Contents
Introduction to Muscle Stiffness
The physical state of having tight, rigid, or difficult-to-move muscles is known as muscle stiffness. While it’s a common experience that most people encounter at some point in their lives, muscle stiffness can be frustrating and limiting.
It can range from a mild feeling of tightness after exercise to severe, painful immobility, potentially affecting daily activities and overall quality of life. Often associated with exercise, muscle stiffness can also occur due to a variety of other factors, such as stress, poor posture, injury, or medical conditions. Whether it’s a short-lived response to physical exertion or a symptom of a more chronic issue, muscle stiffness can lead to significant discomfort and inconvenience.
What Is Muscle Stiffness?
Muscle stiffness refers to an unusual sensation of tightness or resistance in the muscles, where they feel difficult to move or stretch. It can occur in any muscle group, although it is commonly felt in areas like the neck, shoulders, back, and legs. People with muscle stiffness often describe a feeling of being “tight” or “rigid,” with limited mobility or flexibility.
Depending on the severity, it may feel like a mild discomfort or a more intense, painful restriction of movement. While muscle stiffness is most commonly temporary, it can sometimes be a symptom of a more serious underlying issue. The sensation of stiffness is often accompanied by muscle soreness, fatigue, and even swelling in some cases. In extreme forms, it can severely limit a person’s ability to move or perform daily tasks.
Muscles are classified as skeletal, cardiac, or smooth. Skeletal muscle, a consciously controlled muscle type that allows people to move and carry out daily tasks, is the main muscle affected by muscle stiffness. Generally speaking, these actions are made possible when a nervous system signal causes the skeletal muscle to contract, causing movement. The muscles may stay tensed and cause stiffness if there are issues that disrupt the nerve system’s ability to communicate with the muscle cells.
Anatomy of Muscle Function
Muscles are essential components of the human body, responsible for enabling movement, maintaining posture, and performing various physiological functions. The anatomy of muscle function is complex, involving the coordination of muscles, bones, tendons, nerves, and energy systems.
Basic Structure of Muscles
The muscles in the human body are made up of specialized tissue designed to contract and produce force. The anatomy of muscle tissue can be broken down into several hierarchical levels:
Muscle Fibers
The voluntary cells that comprise muscular tissue are called muscle fibers. They can cover a muscle’s whole length and are lengthy, cylindrical cells.
Each muscle fiber is surrounded by a plasma membrane called the sarcolemma and contains several smaller components responsible for muscle contraction.
Myofibrils
Inside apiece of muscle fiber are more smallish thread-like structures named myofibrils, which are formulated of reprising units comprehended as sarcomeres. Myofibrils are the contractile ingredients of muscle fibers.
Sarcomeres, which are made up of thick (myosin) and thin (actin) filaments, are the essential components of muscle contraction. The layout of these filaments delivers muscle fibers their striated impression.
Muscle Fascicles
A muscle fascicle is a bundle of muscle fibers surrounded by a connective tissue layer called the perimysium.
The fascicles are gathered together to create the muscle, which is then covered in a connective tissue termed the epimysium.
Tendons
Tendons, which bind muscles to bones, are thick sheets of connective tissue composed primarily of collagen fibers. Tendons are essential for transmitting force from muscle contractions to bones, which permits body components to move.
Types of Muscles in the Human Body
Muscle tissue comes in three primary varieties, each with unique architecture and purposes:
Skeletal muscle
Affixed to bones, skeletal muscles limit spontaneous movements like carrying objects, running, and stepping. Because of the way the actin and myosin filaments are arranged, these muscles seem striped when viewed under a microscope.
Skeletal muscle fibers are multi-nucleated and can vary in size, depending on the muscle’s function and location.
The somatic nervous system regulates these muscles, which are controlled intentionally.
Internal organ walls, containing those of the stomach, intestines, blood arteries, and bladder, are formulated of smooth muscle. Smooth muscle does not bend and contracts on its own, in contrast to skeletal muscle.
The spindle-shaped smooth muscle fibers have just one nucleus in an independent cell.
The contraction of smooth muscle is responsible for moving food through the digestive tract, regulating blood flow, and other essential functions of internal organs.
Cardiac muscle
The heart possesses respiratory muscle, which is dependable for circulating blood across the body. Cardiac muscle is striated like skeletal muscle, but it is involuntary and has a unique feature: its fibers are connected by intercalated discs, allowing for synchronized heart contraction.
Under the authority of the autonomic nervous system, the heart muscle contracts constantly and regularly without being aware of restrictions.
The process of muscle contraction
Muscle contraction is a highly coordinated process involving the interaction of the nervous, muscle fibers, and energy systems. The fundamental process of muscle contraction is known as the sliding filament theory, which describes how actin and myosin filaments interact to produce force.
Neuromuscular Junction
The nervous system and muscle junction is the term used to describe the middle portion of a muscle fiber and a motor neuron.
When an action potential (electrical signal) reaches the motor neuron. Acetylcholine is a neurotransmitter that is released by the motor neuron. Acetylcholine binds to receptors on the muscle fiber’s sarcolemma, causing an influx of calcium ions into the muscle cell.
Calcium Release and Interaction with Myofilaments
Calcium ions are terminated to initiate the subsequent stage of muscle contraction.The actin filaments’ troponin protein binds to calcium, changing its structure and exposing myosin head binding sites.
After that, the myosin heads create cross-bridges by attaching to the exposed actin filament locations.
Power Stroke
After binding to actin, the myosin heads undergo a conformational change known as the power stroke, which draws the actin filaments toward the sarcomere’s core.
Muscle contraction is caused by the sarcomere being shortened as an outcome. The hydrolysis of ATP gives the energy crucial for the myosin heads to “pivot” and move the actin filaments, concluding in the power stroke.
Detachment and Resetting
After the power stroke, the myosin heads detach from the actin filaments and “reset” to their original position, allowing the cycle to repeat as long as calcium ions are present and ATP is available.
The continuous cycling of cross-bridge formation, power strokes, and detachment leads to the sliding of actin and myosin filaments, which shortens the muscle fiber and causes contraction.
Relaxation
When the signal from the motor neuron stops, calcium ions are actively pumped back into the sarcoplasmic reticulum, a specialized organelle that stores calcium.
As calcium levels drop, troponin and tropomyosin (another protein) cover the binding sites on actin, preventing further interaction with myosin.
As a result, the muscle relaxes and the muscle fiber lengthens back to normal.
Types of Muscle Contractions
Muscles can contract in different ways, depending on the external load and the action being performed. These types of muscle contractions include:
Isometric Contraction: When a muscle contracts isometrically, it renders energy without modifying length. When a muscle contracts against an unmovable object, like when pressing against a wall, something happens. There is no movement even though the muscle is producing stress.
Concentric Contraction: When the muscle decreases while producing force, this is known as a concentric contraction. This type of contraction is common during activities like lifting a weight or performing a bicep curl, where the muscle is working to overcome resistance and shorten during the movement.
Eccentric Contraction: An eccentric contraction occurs when a muscle is prolonged while maintaining force production. This typically happens when the muscle is controlling the descent of a weight or resisting an external force, such as lowering a dumbbell during a bicep curl. Eccentric contractions are responsible for the “negative” phase of many exercises.
Energy Sources for Muscle Contraction
Muscle contraction requires energy, and this energy is primarily derived from the breakdown of ATP.
There are three main systems by which muscles produce ATP:
Phosphagen System: The phosphagen system is the fastest way to produce ATP and is used for short bursts of activity (e.g., sprints, and heavy lifting). This method rapidly regenerates ATP by using muscles’ stored ATP and creatine phosphate.
Glycolytic System: The glycolytic system uses a mechanism known as glycolysis to convert glucose to pyruvate. This system is slower than the phosphagen system but can provide ATP for moderate-intensity activities ranging in duration from 30 seconds to a few minutes. If oxygen is unavailable, pyruvate is converted into lactate, leading to the “burn” often felt during intense exercise.
Oxidative System: The oxidative system is the most efficient system for producing ATP, particularly during long-duration, low-intensity activities like walking or jogging. This system relies on oxygen to fully metabolize glucose and fatty acids to produce ATP in the mitochondria.
Muscle Fiber Types
Three primary categories of muscle fibers are distinguished by their energy systems and rate of contraction:
Type I (Slow-Twitch Fibers)
Slow-twitch fibers comprehended as type I fibers are planned for endurance exercises. They are rich in mitochondria and use the oxidative system to generate ATP. These fibers are perfect for long-distance running since they contract slowly and don’t become tired easily.
Type IIa (Fast-Twitch Fibers)
Type IIa fibers combine characteristics of slow-twitch and fast-twitch fibers to create an intermediate fiber. They exert more force than Type I fibers while being reasonably fatigue-resistant. These fibers are utilized for exercises like weightlifting at a moderate effort or middle-distance running.
Type IIb (Fast-Twitch Fibers)
Fast-twitch fibers of type IIb provide a lot of force efficiently, but they also wear out shortly. They rely on the glycolytic system for energy and are ideal for explosive activities like sprinting or weightlifting.
The Physiology Behind Muscle Stiffness
Muscle stiffness is more than just a physical sensation of tightness or discomfort it’s the result of complex biochemical and mechanical processes that occur within muscle fibers, connective tissues, and the nervous system. To understand why muscles stiffen, it’s helpful to look at the underlying physiology and the body’s response to various stressors, such as exercise, injury, stress, or illness. the mechanisms behind muscle stiffness, focusing on the role of muscle contraction, inflammation, the nervous system, and other key factors that contribute to tightness and reduced mobility.
Muscle Contraction and Relaxation
To understand muscle stiffness, it’s essential to first understand how muscles function. Muscles contract and relax to move. This process involves the interaction between muscle fibers and specialized proteins that allow them to shorten (contract) and lengthen (relax). The key proteins involved in muscle contraction are actin and myosin, which form cross-bridges during contraction.
How Muscle Contraction Works:
Excitation-Contraction Coupling: When a muscle receives a signal from the nervous system (via electrical impulses from motor neurons), calcium ions are released into the muscle fibers. The muscle’s actin and myosin filaments are triggered by this, sliding past one another and contracting.
ATP Exploit: adenosine triphosphate, the energy currency of the body, is mandated for muscle contraction. ATP allows myosin heads to bind to actin and pull, creating tension that leads to movement. ATP also helps muscle fibers relax once contraction is no longer needed.
Muscle Stiffness and Contraction:
When muscles become stiff, they may be stuck in a contracted state, unable to relax properly. This could happen for several reasons, such as inadequate energy (ATP) or excess calcium in the muscle cells.
Stiffness can also occur when the muscle fibers are excessively contracted and remain in that state for an extended period this can lead to a feeling of tightness or rigidity, limiting range of motion.
Microtrauma and Muscle Repair
Muscle stiffness is often linked to muscle damage that occurs during exercise or physical exertion. When muscles are subjected to intense activity, especially unfamiliar or prolonged exercise, the muscle fibers can sustain microscopic tears. This process is referred to as microtrauma and is a key contributor to the feeling of soreness and stiffness that follows exercise.
The Role of Microtrauma in Muscle Stiffness:
Inflammation Response: After muscle fibers are damaged, the body initiates an inflammatory response. White blood cells and inflammatory cytokines (such as prostaglandins and interleukins) rush to the affected area to begin the repair process. Inflammation increases the volume of fluid in the muscle tissue, causing swelling and stiffness.
Domination of Eccentric Movements: Eccentric movements where muscles lengthen while contracting, such as during the lowering phase of a squat or when running downhill—are particularly associated with microtrauma. These movements generate higher amounts of force and can cause more damage to the muscle fibers, leading to increased stiffness, soreness, and delayed onset muscle soreness (DOMS).
Healing Process and Stiffness:
As the muscle repairs itself, new muscle fibers are created, which helps the muscle grow stronger over time. nevertheless, the muscle may feel rigid, achy, and sensitive to the touch throughout this healing stage. The stiffness is temporary and will typically subside as the healing process progresses and inflammation decreases.
Scar Tissue Formation: In some cases, if the muscle sustains more significant damage, scar tissue may form as part of the healing process. If left untreated, this scar tissue may cause tightness and decreased flexibility over time.
Neural Adaptation and Stiffness
The nervous system adapts to prolonged stress, overuse, or injury by increasing the baseline level of muscle tone, a condition known as hypertonia. This can be a protective mechanism in response to injury, inflammation, or the body’s attempt to prevent further damage. However, if the muscle stays in a heightened state of tension, it can lead to long-term stiffness and discomfort.
Psychological factors, such as stress and anxiety, can also amplify muscle stiffness. Muscle contraction, especially in the shoulders, neck, and back, results from the sympathetic nervous system being activated by the body’s stress reaction. Over time, this can create a feedback loop where mental stress results in increased physical tension, further exacerbating muscle stiffness.
The Nervous System’s Role in Muscle Stiffness
The nervous system plays a central role in the regulation of muscle tone and stiffness. Both voluntary and involuntary nervous system processes contribute to the sensation of muscle tightness.
Muscle Spindles and Golgi Tendon Organs
Specialized sensors called muscle spindles are found inside muscles and are responsible for detecting variations in muscle length and stretching velocity. Muscle spindles communicate with the spinal cord when a muscle will contract instinctively if it is stretched too quickly or too much. This process is called the stretch reflex. While this reflex can help prevent injury, it can also contribute to a feeling of tightness if the muscle is continuously stretched or overused.
Sensory receptors found in tendons called Golgi Tendon Organs (GTOs) keep track of the amount of force or stress that the muscles are exerting.GTOs instruct the spinal cord to relax muscles when tension becomes too much. In cases of muscle overuse, these receptors can contribute to the feeling of tightness, as the muscle is under constant tension.
Inflammation and Swelling
Inflammation is a key physiological response that leads to muscle stiffness. While it is essential for the healing process, inflammation can also contribute to the sensation of tightness and discomfort in the muscles.
Acute Inflammation
Prostaglandins and other inflammatory mediators are released when tissue damage occurs, causing blood vessels to dilate and increasing the permeability of the blood vessel walls. This allows immune cells to enter the affected area and start the repair process. However, this increased fluid accumulation in the muscle tissue can cause swelling, which leads to a feeling of tightness. The combination of swelling and increased blood flow to the area also increases the sensitivity of nerve endings, contributing to the feeling of stiffness and pain.
Chronic Inflammation
In cases of chronic overuse, injury, or certain medical conditions (such as arthritis), inflammation may persist for longer periods, leading to ongoing stiffness and discomfort. Chronic inflammation can also lead to muscle fatigue and weakness, as the muscles are under constant stress.
Cytokines and Pain Sensitivity: Inflammatory cytokines, such as TNF-alpha and interleukins, sensitize the nervous system, making the muscles and surrounding tissues more sensitive to pain. This can heighten the feeling of muscle stiffness, especially during movement or when pressure is applied to the affected area.
The Role of hydration and electrolytes
Muscle function and stiffness are also significantly influenced by electrolyte balance and hydration. Electrolytes like sodium, potassium, calcium, and magnesium are vital for proper muscle contraction and relaxation. When these electrolytes are out of balance, either due to dehydration, inadequate nutrition, or excessive sweating, it can impair muscle function and contribute to stiffness.
Calcium Imbalance: Calcium ions play a key role in the muscle contraction process. If calcium levels are too high in the muscle cells, muscles can remain contracted and stiff. On the other hand, weak or uncoordinated muscular contractions may result from low calcium levels.
Magnesium Deficiency: Magnesium helps muscles relax after contraction. A magnesium deficiency can result in muscle cramps, tightness, and stiffness, especially after exercise.
Dehydration: When the body is dehydrated, the muscles are more likely to cramp and stiffen. Adequate hydration helps maintain electrolyte balance, ensuring that muscles can contract and relax properly.
Long-Term Adaptations and Muscle Stiffness
In the long term, muscle stiffness can occur due to changes in muscle and connective tissue structure. For example:
Muscle Shortening and Fibrosis: When muscles are kept contracted for extended periods, such as from poor posture or repetitive stress, they can become shortened and less flexible. This can lead to a condition called fibrosis, where scar tissue builds up in the muscle, further limiting movement and increasing stiffness.
Tendon and Ligament Stiffness: Chronic muscle stiffness can also affect the tendons and ligaments surrounding the muscles. Over time, connective tissues may become stiffer, making it harder for the muscles to move freely
The Different Forms of Muscle Stiffness
Muscle stiffness can vary significantly in its form and intensity, depending on its cause. Here are a few common types of muscle stiffness that people experience:
Acute muscle stiffness
Acute muscle stiffness is typically short-term and is often experienced after physical exertion, especially following activities that involve unfamiliar or intense physical activity. Delay in onset muscle soreness (DOMS), which peaks 24 to 48 hours after activity, is most frequently linked to it.
Causes of acute muscle stiffness
Intense exercise or physical activity: Engaging in strenuous activity or exercise that your body is not accustomed to, such as lifting heavy weights, running long distances, or doing vigorous sports, can lead to muscle stiffness.
Muscle microtears: During intense exercise, tiny tears occur in muscle fibers, which results in the stiffness and soreness often felt in the 24–48 hours post-workout.
Lactic acid buildup: Although it is not the primary cause, during intense physical exertion, lactic acid can accumulate in the muscles and contribute to temporary tightness or stiffness.
Symptoms
- a feeling that the muscles are painful or tight.
- Restricted movement or range of motion.
- Mild to moderate discomfort, especially when stretching or moving the affected muscle.
Stress-related muscle stiffness
Mental and emotional stress can trigger the body’s “fight-or-flight” response, which leads to muscle tension. This type of stiffness often manifests in areas like the neck, shoulders, and jaw. It can result in chronic pain and discomfort if not managed, as continuous stress may cause the muscles to remain contracted for extended periods.
Muscle Stiffness from Injury or Overuse
Muscle strains, sprains, or overuse injuries can result in stiffness in the affected area. This stiffness can be a result of inflammation as the body tries to heal the injury. In addition to the stiffness, there may be discomfort, edema, and bruises.
Chronic muscle stiffness
Conditions such as fibromyalgia, arthritis, and neurological disorders like Parkinson’s disease can cause ongoing muscle stiffness. In these cases, stiffness may not only be a result of muscle overuse or stress but also due to underlying health conditions that affect the muscles and joints directly. Chronic muscle stiffness refers to long-term tightness or discomfort in the muscles that lasts for weeks or months. It is often more persistent than acute stiffness and may be associated with overuse, poor posture, or underlying medical conditions.
Symptoms
- Tightness in the muscles that persists for weeks or months
- Decreased flexibility and range of motion.
- Dull, aching pain that worsens with activity or prolonged static positions.
- Difficulty in performing normal daily activities due to discomfort.
Postural muscle stiffness
Poor posture, especially when sitting for long periods or standing in improper alignment, can lead to stiffness. Muscles that are held in one position for extended periods can become tight, sore, and weakened. This is commonly seen in individuals who work long hours at desks or those who don’t engage in regular physical activity.
Symptoms
- difficulty maintaining proper posture over extended periods.
- restricted mobility in the afflicted regions.
Inflammatory Conditions
Certain medical conditions that cause inflammation can lead to muscle stiffness as part of the overall symptoms. Conditions like arthritis, autoimmune diseases, and infections may cause muscle stiffness as the body’s immune system targets joints or tissues.
Causes of Inflammatory Muscle Stiffness
- Rheumatoid Arthritis (RA): An autoimmune condition that causes inflammation in the joints, leading to stiffness and pain in the muscles surrounding the affected joints.
- Osteoarthritis (OA): A degenerative joint disease that can result in muscle stiffness, particularly in the hips, knees, and lower back, due to the wear and tear of cartilage.
- Infections: Some viral or bacterial infections, such as the flu or Lyme disease, can lead to muscle aches and stiffness as part of the body’s immune response.
- Myositis: Inflammation of the muscles, often caused by autoimmune diseases, infections, or medications, can result in muscle weakness and stiffness.
Symptoms
- prolonged tightness of the muscles in particular body parts.
- Alongside the rigidity, there may be joint pain and swelling.
- poor ROM because stress muscles
- General fatigue and malaise, especially in inflammatory diseases.
Muscular Spasms and Cramps
An uncontrollable contraction of a muscle that results in abrupt, intense pain and stiffness is called a muscle spasm. Cramps are a type of spasm that typically occur in the legs or feet, often at night or during physical activity. Muscle stiffness can be caused by cramps or spasms.
Causes of Spasms and Cramps
Dehydration: Lack of sufficient fluids can lead to muscle cramps, especially in hot weather or during exercise.
Electrolyte Imbalance: Low levels of important electrolytes like potassium, calcium, or magnesium can disrupt normal muscle function and cause spasms.
Overexertion: Pushing muscles beyond their normal limits, especially during intense or prolonged physical activity, can result in spasms.
Poor Circulation: Conditions that affect blood flow, such as peripheral artery disease, can contribute to cramps and spasms.
Nerve Compression: Nerve impingements in the spine, such as a herniated disc, can lead to muscle spasms in the affected areas.
Symptoms
- The afflicted muscle feels suddenly tight and painful.
- A visible “knotted” appearance of the muscle, is often accompanied by swelling.
- restricted range of motion in the joint or muscle that is impacted.
- The feeling of the muscle being “locked” in a contracted position.
Causes of Muscle Stiffness
Exercise-induced Muscle Stiffness
Muscle stiffness is frequently brought on by exercise or other physically demanding tasks. Stiffness frequently happens when someone begins a new fitness program or regimen, or when they increase the length and intensity of their existing routine. This results in tiny damage to the muscle fibers, which makes the muscles work harder and makes them stiff or sore. Delay in onset muscle soreness (DOMS) is another term for this kind of injury.
Exercise-induced muscle stiffness is primarily caused by microscopic damage to the muscle fibers, a process that is especially common in intense or unfamiliar exercise. The following are the main causes of muscular stiffness:
Microtrauma (Microtears)
Inflammatory Response: Following microtears, the body initiates an inflammatory process to repair the damaged muscle fibers. Inflammation causes an increase in fluid and white blood cells in the affected tissue, leading to swelling, tenderness, and the feeling of tightness or stiffness.
Tissue Repair and Growth: While muscle repair occurs, new muscle tissue is laid down, making the muscle stronger. However, during this healing process, the muscles may feel sore and stiff, which is part of the body’s natural recovery mechanism.DOMS can be brought on by any movement although it is frequently brought on by jogging or running downhill, using weights, doing squats, doing push-ups
The Role of eccentric exercise in muscle stiffness
Eccentric exercises are a primary contributor to exercise-induced muscle stiffness and soreness. In eccentric movements, muscles are lengthened while under tension, which places more stress on the muscle fibers compared to concentric movements, where the muscles shorten.
An eccentric contraction occurs when a muscle resists the force while lengthening. For example, when you lower a dumbbell in a bicep curl or descend a staircase, your muscles are working eccentrically.
Eccentric Exercise Examples: Running downhill, performing negative repetitions (slow lowering phase) during strength training, and certain activities like jumping or plyometrics all involve eccentric muscle actions.
Eccentric Contractions and Muscle Stiffness
Eccentric movements cause a higher level of mechanical stress on muscle fibers, resulting in more microtrauma compared to concentric movements. The increased strain on the muscle leads to more inflammation and swelling as part of the repair process, which contributes to muscle stiffness and soreness.
The severity of DOMS and muscle stiffness is generally greater after eccentric exercise because these movements require the muscles to generate force while elongating. This dynamic places greater strain on the muscle fibers, leading to more pronounced muscle stiffness.
Delayed Onset Muscle Soreness (DOMS)
A particular type of muscle stiffness called DOMS usually manifests 12 to 24 hours after activity and peaks 48 hours later. It is most commonly associated with intense or unfamiliar exercise, particularly activities that involve eccentric movements.
Eccentric Movements: Eccentric contractions occur when a muscle lengthens under tension, such as when lowering a weight during a bicep curl or walking downhill. These types of contractions cause more strain on the muscle fibers, leading to a higher likelihood of microtears and soreness.
DOMS is often characterized by stiffness, tenderness, and reduced range of motion. It is typically harmless and a normal part of muscular adaptation, even if it can be uncomfortable.
intensity and duration of exercise
The intensity and duration of physical activity play a crucial role in the severity of muscle stiffness. High-intensity exercise, especially when combined with heavy weights or prolonged duration, can cause more muscle strain and more microtears. In these cases, the body requires more time to repair the muscle tissue, which leads to greater stiffness.
Intensity Factors: Exercises that require maximal effort or involve high resistance tend to place a lot of strain on the muscles. When muscles are pushed beyond their normal capacity, such as during heavy lifting or sprinting, there is a higher risk of muscle damage, resulting in greater stiffness.
Lack of Warm-up and Cool-down
A proper warm-up before exercise helps prepare the muscles for physical activity by increasing blood flow, oxygen delivery, and flexibility. Without a warm-up, muscles are more likely to become tight and stiff due to insufficient preparation.
Cool-down and Stretching: After exercise, cooling down with gentle movements and static stretching helps return the muscles to their normal length and promotes relaxation. Without adequate stretching post-exercise, muscles may remain tight and stiff as the body may not return to its pre-exercise state effectively.
Inflammatory Response
When muscle fibers sustain microtears, the body starts with the healing task by inducing an inflammatory response. This response involves the release of inflammatory chemicals like prostaglandins and cytokines, which increase blood flow to the affected muscles and attract white blood cells to the injury site. While this inflammation is necessary for healing, it contributes to the sensation of soreness and stiffness.
Edema: The increased fluid retention around the damaged muscle fibers can cause edema, or swelling, which further limits the muscle’s flexibility and contributes to pain and tightness
Metabolic Byproducts: During exercise, especially high-intensity activity, the body produces metabolic byproducts like lactic acid. These byproducts build up in the muscles and contribute to the initial discomfort or “burn” felt during the workout. While lactic acid itself does not cause DOMS, it can exacerbate the pain during and immediately after exercise.
Structural damage: DOMS can cause damage to tendons and sarcomeres, the fundamental contractile units found in muscle fibers, in addition to small tears in muscle fibers. Muscle discomfort and stiffness are further exacerbated by this structural damage, which also increases the inflammatory response.
Strains and Sprains
Sprains and strains, which can impact both the muscles and ligaments, are the most frequent cause of muscle stiffness.
The term “strain” refers to the tearing or straining of muscle fibers. The lower back and legs are frequently strained.
A sprain occurs when the ligaments are ripped, twisted, or stretched.
Typical sprain-prone locations include: ankles, wrists, thumbs, and knees
Rheumatic polymyalgia
Rigidity and redness in the muscles are symptoms of polymyalgia rheumatica. The upper body, which includes the arms, neck, and shoulders, is typically affected. It frequently affects the hips as well. A person with polymyalgia rheumatica is typically 70 years old, while some people may not have it until they are in their 80s.
The following are further signs of polymyalgia rheumatica: Problems falling asleep Having trouble putting on clothes shifting posture, such as getting out of a car or chair
Stings or bites
Muscle stiffness can occasionally result from insect bites and stings. A red, swelling lump on the skin that is unpleasant and itching can also be caused by bites or stings. The following insects frequently bite or sting and can make muscles stiff:
- Hornets and wasps
- Bees
- Ticks, horseflies, and mosquitoes
- Midges, fleas, and spiders
Although most bite or sting symptoms go away in a few days, some people experience allergic reactions that can necessitate medical care. More severe illnesses like Lyme disease, malaria, or Rocky Mountain spotted fever can also be linked to stiffness following an insect bite. These disorders will also bring other symptoms, such as fever and malaise.
Infections
Furthermore, to other symptoms, certain illnesses produce stiffness in the muscles. Among these infections are: HIV, polio, influenza, tetanus a bacterial illness usually affixed with soil or dirt, meningitis a brain and spinal cord infection
Injury
This leads to the most extensive soft tissue damage in the tendons, ligaments, and muscles. These may happen when exercising, playing sports, or performing daily tasks.
Soft tissue injuries can take two different forms:
Acute injuries must result from a brief impact on the body, a fall, or a twisting.
Overuse issues might arise from performing an activity so frequently that the muscles don’t have adequate time to rest in between repetitions. Overuse injuries might include bursitis and tendinitis.
Both the degree of injuries and the concurrent symptoms might deviate. Apart from a sensation of constriction or rigidity, additional potential symptoms consist of: cramps, pains, spasms, discomfort, edema, and weakness
Lupus
An autoimmune condition named lupus must simulate nearly any organ in the body. Periods of remission, when symptoms may improve, and flare-ups, when symptoms intensify, are both possible outcomes of the illness.
Each person may experience lupus symptoms differently. Other potential lupus symptoms, in addition to muscle stiffness, include:
- joint or muscle ache
- Chest pain, rash, fever, light sensitivity, hair loss, and anemia
- extended weariness
- mouth sores
- kidney issues
- memory problems
Lyme illness
The most prevalent vector-borne illness in the US is this one.
Lyme disease can produce several symptoms, such as stiff necks and muscle aches and pains if treatment is not received.
Other signs and symptoms could be:
- headache, exhaustion, chills, fever, enlarged lymph nodes, rash, joint discomfort, and swelling
- Heart palpitations or an irregular heartbeat
- shortness of breath episodes
- instances of lightheadedness
infectious mononucleosis
Teenagers, young adults, and college students are frequently afflicted with contagious mononucleosis.
Not every symptom will appear at once, and others may appear steadily over time. Other potential symptoms, in addition to muscle pains and stiffness, include: rash, headache, sore throat, excessive exhaustion, raised spleen, lengthened liver and lymph nodes
Some people’s symptoms may go away in two to four weeks, while others may still have them weeks or months later.
Having fibromyalgia
All over the body, fibromyalgia can cause excruciating discomfort.
In addition to pain and stiffness that can occur anywhere on the body, fibromyalgia symptoms also include:
- exhaustion
- Problems sleeping
- migraine or headache anxiety
- depression and cognitive issues
- absorb issues, facial or jaw pain, and unemotional or stinging hands and feet
Stress and Anxiety
Mental stress can have a profound impact on physical health, and one of the most common effects is muscle stiffness. When the body is under stress, the sympathetic nervous system is activated, causing muscles to contract in preparation for “fight or flight.” Chronic stress can lead to prolonged tense muscles, frequently in the neck, shoulders, and lumbar back.
Stress and Anxiety-Induced Muscle Tension
Muscle tension caused by stress and anxiety is a common phenomenon that affects individuals across various age groups. This type of muscle stiffness or tightness occurs when the body responds to psychological stress by activating the “fight-or-flight” response, which can result in physical symptoms such as muscle tightness, discomfort, and pain.
The Physiological Mechanism of Muscle Tension
When the body perceives a threat or stressor, the brain releases stress hormones like adrenaline (epinephrine) and cortisol. These hormones signal various systems in the body to prepare for immediate physical action.” Numerous physiological alterations are brought about by this remedy, involving:
Increased heart rate: This enables the heart to pump blood more quickly, providing oxygen and nutrition to muscles.
Elevated blood pressure: This helps ensure that blood flows quickly to vital organs and muscles in response to the stressor.
Tensing of muscles: Muscles throughout the body tighten as part of the body’s readiness to either fight or flee. In places like the neck, shoulders, jaw, and back, this is very apparent.
Muscles are designed to contract and relax efficiently. However, when the body remains in a constant state of stress or anxiety, muscles can stay in a contracted state, leading to persistent muscle tension. Over time, this can cause pain, and discomfort, and even contribute to muscle injury.
Areas Most Affected by Stress and Anxiety-Induced Muscle Tension
Certain muscle groups in the body are more prone to becoming tense under stress and anxiety. The areas most commonly affected include:
- Neck and Shoulders: One of the most common areas where stress-related muscle tension manifests. People under stress or anxiety often carry tension in their upper body, leading to tightness and discomfort in the neck, shoulders, and upper back.
- Jaw and Facial Muscles: Clenching the jaw, grinding teeth, or frowning are common responses to stress and anxiety. This may result in temporomandibular joint (TMJ) issues, headaches and migraines, and pain in the jaw.
- Back Muscles: The lower back, particularly the lumbar area, is also susceptible to tension from stress. Chronic anxiety can contribute to stiffness and discomfort in the lower back, sometimes leading to issues like muscle spasms or poor posture. Arms and Hands: Muscle tension can also occur in the arms and hands, particularly if a person is holding themselves rigidly during stressful situations. This can cause discomfort or lead to repetitive strain injuries.
- Chest and Abdominal Muscles: The chest and abdominal regions can tighten as part of the body’s fight-or-flight response. This can cause shallow breathing, discomfort, or even sensations of tightness in the chest that mimic cardiac symptoms.
Symptoms of stress and anxiety-induced muscle tension
The symptoms of muscle tension caused by stress and anxiety can range from mild to severe. These symptoms may include:
- Persistent tightness or stiffness: Individuals often report feeling like their muscles are “locked” or “stiff,” even when not engaging in physical activity.
- Pain or discomfort: Muscle tension can cause localized pain, which may worsen with movement or over time if left unaddressed.
- Headaches: Tension headaches, often associated with tightness in the neck and shoulders, are common in those experiencing stress and anxiety. Most people describe these headaches as feeling like a band constricting around their head.
- Jaw clenching or teeth grinding: Known as bruxism, this behavior often occurs during sleep or while awake due to anxiety, leading to pain in the jaw and facial muscles.
- Reduced range of motion: Muscle tension can limit the flexibility and mobility of affected areas. For example, tight shoulders or neck muscles can make it difficult to turn the head or perform certain movements.
Impact of stress and anxiety-induced muscle tension on daily life
Muscle tension caused by stress and anxiety can have wide-reaching effects on a person’s daily life. Chronic muscle tightness and pain can interfere with normal physical activity, work performance, and social interactions.
- Reduced mobility: Persistent muscle tension can limit a person’s range of motion, making it difficult to perform everyday tasks such as turning the head, lifting objects, or even sitting for long periods.
- Chronic pain: If left untreated, muscle tension can contribute to long-term pain and discomfort. This can influence sleep, mood, and overall quality of life.
- Mental health impact: The pain and discomfort from muscle tension can further exacerbate stress and anxiety, creating a vicious cycle where the physical symptoms reinforce the emotional distress.
- Decreased productivity: Tension in the muscles can lead to fatigue and a reduced ability to focus or engage in work-related tasks, which can impact job performance and overall satisfaction.
Sedentary lifestyle and poor posture relation with muscle stiffness
Muscle stiffness can result from inactivity and extended periods of inactivity. Sitting for extended periods, especially in poor posture, places strain on certain muscle groups. Over time, muscles that are not regularly stretched or exercised can become tight, weak, and stiff. This is particularly common in people who work at desks or live relatively sedentary lives.
Poor posture and a sedentary lifestyle are two widespread health issues that often go hand in hand, contributing to a variety of physical and psychological problems. These habits are increasingly common in the modern world, especially with the rise of desk jobs, excessive screen time, and the general decline in physical activity.
Understanding Poor Posture
The posture is understood to be the curve of the body, whether it is any position like standing, sitting, or lying down. Proper posture involves maintaining the natural curvature of the spine, which includes the cervical (neck), thoracic (upper back), and lumbar (lower back) curves. Proper posture ensures that the body’s weight is distributed evenly, allowing muscles and joints to function efficiently and minimizing the risk of strain.
Poor posture, on the other hand, refers to any misalignment of the body that places undue stress on the spine, muscles, and joints. It often occurs when the natural curves of the spine are altered due to habits or environmental factors. Some of the most standard types of poor posture comprise:
- Slouching: A forward head and rounded shoulders that place excessive strain on the neck and upper back muscles.
- Forward head posture: A condition where the head juts forward, typically due to prolonged screen time or poor ergonomic setups.
- Kyphosis: An excessive rounding of the upper back, often seen in older adults or those with poor sitting habits.
- Lordosis: An exaggerated inward curve of the lower back, which can occur due to sitting for extended periods without proper lumbar support.
The sedentary lifestyle epidemic
Long stretches of inactivity, frequently spent sitting or lying down, with little to no physical action, are indicative of a lifestyle that is sedentary. This is increasingly common in modern society due to technological advancements, such as the widespread use of computers, smartphones, and television, combined with the convenience of cars and automated services.
The rise of sedentary behavior, especially in work and leisure, has created a culture where many people are spending hours sitting without regular physical activity. Adults in wealthy nations spend almost half of their waking hours sitting. This shift in lifestyle has significant consequences for both physical and mental health.
The link between poor posture and sedentary lifestyles
While poor posture and a sedentary lifestyle are separate issues, they are intrinsically linked, often amplifying each other. The more time spent sitting or in a sedentary position, the more likely poor posture will develop. In turn, poor posture can worsen the effects of a sedentary lifestyle, creating a cycle of discomfort, pain, and reduced mobility. When a person spends prolonged periods sitting with improper posture, the muscles that support the spine become weak and fatigued. Additionally, the muscles that are stretched during sitting such as the hip flexors become tight, leading to muscle imbalances that further contribute to poor posture.
Physical consequences of poor posture and sedentary living
The combination of poor posture and a sedentary lifestyle can lead to a variety of physical problems, ranging from mild discomfort to chronic pain and long-term damage. Among the most prevalent problems are:
Musculoskeletal Pain
- Back Pain: One of the most common complaints associated with poor posture and prolonged sitting is lower back pain. Sitting for long periods, especially with poor lumbar support, can cause the spine to become misaligned, leading to muscle strain and discomfort.
- Neck and Shoulder Pain: Poor posture, especially forward head posture, can place excessive strain on the neck and shoulder muscles, leading to tension, pain, and even headaches.
- Joint Problems: Prolonged sitting can also affect joint health, leading to stiffness in the hips, knees, and ankles. The lack of movement can reduce the joint’s range of motion and lead to the deterioration of cartilage over time.
Muscle imbalances
- Weak Core Muscles: Sitting for long hours weakens the core muscles that support the spine, including the abdominals, obliques, and lower back muscles. Back pain and bad posture can both be made worse by a weakened belly.
- Tight Hip Flexors and Hamstrings: When sitting, the hip flexors (muscles at the front of the hips) are shortened, and the hamstrings (muscles at the back of the thighs) become lengthened. This can lead to tightness and discomfort in both areas, affecting posture and movement.
- Weak Gluteal Muscles: Sitting for long periods also weakens the gluteal muscles (buttocks), which are important for stabilizing the pelvis and supporting proper posture. Powerless glutes should conduct compensatory motions in the lower back and hips.
Decreased mobility and flexibility
With a sedentary lifestyle, the body’s natural range of motion can decrease due to muscle stiffness and joint immobility. People who sit for long periods may experience difficulty moving freely, bending over, or reaching for objects without discomfort. This reduced mobility over time may cause posture and physical health to worsen even more.
Increased risk of chronic conditions
Prolonged sitting and poor posture are also linked to an increased risk of several chronic health conditions, including:
- Cardiovascular Disease: Sedentary behavior has been associated with an increased risk of heart disease, high blood pressure, and poor circulation. The lack of movement can negatively affect the cardiovascular system, leading to weight gain, higher cholesterol, and poor blood flow.
- Type 2 Diabetes: A sedentary lifestyle can impair the body’s ability to regulate blood sugar, contributing to insulin resistance and an increased risk of type 2 diabetes.
- Obesity: Lack of movement combined with poor dietary habits often leads to weight gain and obesity. Sitting for long periods decreases energy expenditure and encourages unhealthy eating behaviors.
Mental health issues
Increased Stress: Poor posture can contribute to muscle tension, which, in turn, may increase stress levels. A sedentary lifestyle can also contribute to higher levels of anxiety and depression, as physical activity is known to release endorphins that improve mood.
Reduced Cognitive Function: Physical inactivity has been shown to reduce cognitive function and concentration. A sedentary lifestyle can impair the ability to focus, think clearly, and be productive throughout the day.
Fatigue: Ironically, the more one sits, the more tired they may feel. Sedentary behavior leads to poor circulation and muscle atrophy, which can leave the body feeling sluggish and exhausted.
Aging
As people age, they often experience changes in muscle function, including increased muscle stiffness. This condition, while common in older adults, is not a normal part of aging and can have significant impacts on mobility, flexibility, and overall quality of life. Muscle stiffness in aging individuals can result from a combination of physiological changes, lifestyle factors, and underlying health conditions. Understanding the connection between muscle stiffness and age is essential for managing this condition and maintaining physical independence in later years.
Muscle stiffness with age
Muscle stiffness in older adults is a multifactorial condition, influenced by natural aging processes as well as environmental, lifestyle, and health factors.
Sarcopenia (Age-Related Muscle Loss)
Muscle Mass Decline: One of the primary causes of muscle stiffness with age is sarcopenia, which refers to the gradual loss of muscle mass and strength that occurs as people age. This method naturally initiate near the age of 30 and accelerates after the age of 60. As muscle fibers decrease in number and size, the remaining muscle tissue becomes less efficient, leading to reduced flexibility and increased stiffness.
Muscle Fibers and Function: Older adults experience a loss of fast-twitch muscle fibers, which are responsible for quick, powerful movements. The remaining slow-twitch fibers, which are more endurance-oriented, may not provide the same range of motion and adaptability, resulting in muscle tightness and stiffness, particularly in the legs, back, and shoulders.
Changes in Connective Tissue
Collagen Accumulation: As the body ages, connective tissues like tendons and ligaments become stiffer and less elastic due to an increase in collagen production. Collagen fibers become thicker and less pliable over time, leading to a reduction in the flexibility of muscles and joints. This can contribute to a feeling of muscle tightness, particularly in the morning or after periods of inactivity.
Decreased Synovial Fluid: The joints of older individuals tend to produce less synovial fluid, which acts as a lubricant, reducing friction and supporting smooth joint movement. A decrease in this fluid can cause stiffness and discomfort in the surrounding muscles, making movement more difficult.
Reduced Blood Flow and Oxygen Delivery
Circulatory Changes: Aging leads to changes in the cardiovascular system, including reduced blood flow and the ability to efficiently deliver oxygen and nutrients to muscle tissue. Poor circulation can result in tightness and stiffness in muscles, as they are deprived of the oxygen and nutrients necessary for optimal function and recovery.
Slower Recovery: Reduced circulation also means slower muscle repair and recovery, which can prolong feelings of stiffness and soreness after physical activity.
Changes in the Nervous System
Slower Neural Responses: The aging process affects the nervous system, slowing down the transmission of electrical signals between the brain and muscles. This results in slower muscle contractions and reduced coordination, which can make muscles feel tighter or more resistant to movement.
Decreased Flexibility: The loss of muscle elasticity and the inability of muscles to react quickly can lead to decreased flexibility, increasing the sensation of stiffness. This can be especially noticeable in the neck, lower back, and hamstrings.
Decreased Physical Activity
Sedentary Lifestyle: As people age, they tend to become less active due to various factors such as joint pain, fatigue, and a general decrease in motivation to exercise. A sedentary lifestyle leads to muscle deconditioning and tightness, as muscles that are not regularly used or stretched can become stiff and less flexible over time.
Impact of Inactivity: Without regular physical activity, muscles lose their range of motion, flexibility, and strength. Stiffness may be more pronounced after periods of sitting or lying down, such as in the morning upon waking up.
Osteoarthritis and Other Joint Disorders
Joint Wear and Tear: Osteoarthritis, a degenerative joint disease that becomes more common with age, can cause stiffness in both the muscles and joints. The loss of cartilage and the narrowing of joint spaces in conditions like osteoarthritis can cause the surrounding muscles to become tense and stiff due to the increased strain placed on them.
Inflammation and Pain: Arthritis and other joint conditions can cause inflammation and pain, leading to compensatory muscle stiffness as the body tries to reduce movement to protect the affected joint.
Hormonal Changes
Hormones like estrogen and testosterone, which help maintain muscle mass, decrease with age. This hormonal shift accelerates the loss of muscle tissue, leading to weaker, stiffer muscles. Estrogen, for instance, plays a role in the flexibility and elasticity of tendons and ligaments, and its decrease in postmenopausal women may contribute to the development of stiffness in muscles and joints.
Reduced Muscle Fiber Elasticity
Over time, muscle fibers lose some of their ability to stretch and recoil. Collagen in the connective tissue surrounding muscles increases, causing the tissue to become stiffer and less flexible. This leads to a reduced range of motion and stiffness in the muscles.
Changes in Muscle Composition
The balance of muscle fiber types shifts with aging. Fibers with slow twitch are more focused on endurance, whereas fast-twitch fibers, which are in charge of explosive actions, deteriorate more quickly. This change can reduce the ability to perform rapid movements and increase the feeling of stiffness after physical activity.
Reduced Blood Flow
Aging leads to changes in the cardiovascular system, reducing blood flow to the muscles. Poor circulation can hinder the delivery of oxygen and nutrients to muscle tissue, slowing down recovery and contributing to stiffness, fatigue, and a longer recovery time after exertion.
Decreased Production of Synovial Fluid
As people age, their body produces less synovial fluid, which lubricates the joints. This reduction leads to friction and stiffness in the joints, which can also contribute to muscle stiffness, especially around areas like the knees, hips, and shoulders.
Physical Overexertion
Physical overexertion refers to the excessive physical strain or effort that exceeds the body’s normal capacity, often leading to muscle fatigue, soreness, and stiffness. This condition is common among athletes, individuals engaging in intense exercise, and even those who overdo physical tasks outside of a fitness routine. Muscle stiffness caused by overexertion typically presents as a result of pushing the body too hard without adequate rest or preparation.
Mechanisms behind muscle stiffness from overexertion
When muscles are subjected to excessive physical exertion, several physiological processes are triggered, resulting in muscle stiffness. The mechanisms behind muscle stiffness from overexertion are primarily tied to muscle microtrauma and metabolic byproducts.
Microtears and Muscle Damage
Muscle fiber microtrauma: During intense exercise, particularly eccentric movements (where muscles lengthen under tension, such as during the downward phase of a squat or a running stride), small tears occur in muscle fibers. These microtears are part of the muscle-building process, but they can also lead to muscle soreness and stiffness as the fibers heal.
Inflammation: Microtears in muscle fibers result in an inflammatory response. Inflammation leads to the release of chemicals such as prostaglandins and histamines, which cause blood vessels to dilate, bringing more fluid into the affected area. This fluid accumulation can contribute to swelling, pain, and tightness in the muscles.
Lactic acid buildup
During intense exercise, the body relies on anaerobic metabolism to produce energy when oxygen supply to muscles is insufficient. A consequence of this method is the creation of lactic acid. While lactic acid is not the primary cause of muscle soreness (delayed onset muscle soreness or DOMS), it can temporarily contribute to muscle tightness and discomfort during and immediately after physical exertion.
Lactic acid accumulation: High-intensity exercise without adequate rest causes the body to produce more lactic acid, which can lower the pH in the muscles and contribute to the sensation of stiffness and discomfort. However, the body clears lactic acid relatively quickly post-exercise.
dehydration and electrolyte imbalance
Fluid Loss: Intense physical exertion causes sweating, which results in fluid loss. If hydration levels aren’t adequately replenished, the muscles may experience cramps, spasms, and stiffness due to a lack of adequate water to maintain muscle function.
Electrolyte Imbalance: Muscles need a balance of electrolytes like sodium, potassium, and calcium to function properly. Intense exercise, particularly in hot conditions, can lead to an imbalance in these electrolytes, causing muscles to become stiff or cramp.
Impact of Muscle Stiffness on daily life
Difficulty with Routine Activities
- Bending and Reaching: Simple tasks like bending down to tie shoes, picking up objects from the floor, or reaching for items on a high shelf can become challenging when muscles in the back, legs, or shoulders are stiff.
- Walking and Climbing Stairs: Stiffness in the lower body, particularly in the hips, knees, or ankles, can make walking or climbing stairs painful. This may cause slower movements, fatigue, and a greater risk of falls.
- Joint Stiffness: Muscle stiffness often affects the surrounding joints. For example, tightness in the neck or shoulders can limit head movement, making it hard to look over your shoulder when driving or performing tasks that require full arm extension, such as reaching for something above the head.
- Limited Mobility: Stiffness can affect walking posture and gait. Individuals may adopt compensatory movements, such as limping or walking slowly, which can exacerbate muscle stiffness and lead to further joint problems over time.
- Reduced Athletic Performance: Athletes or those who engage in regular exercise may find that muscle stiffness limits their performance. Tight muscles can lead to less explosive power, reduced strength, and slower recovery after physical exertion, making it harder to meet fitness goals or complete workouts effectively.
- Decreased Endurance: Muscles that are stiff become fatigued more quickly. This reduces overall endurance, making it harder to engage in sustained activities like running, cycling, or swimming.
- Manual Labor: Individuals who perform physical labor—such as lifting, carrying, or repetitive motions may find that stiffness in the muscles, particularly in the back, arms, and legs, hampers their ability to work efficiently and safely. Chronic stiffness can also lead to more frequent injury, further compromising work performance.
- Desk Jobs: On the flip side, those who work in sedentary jobs can experience stiffness in the neck, back, and shoulders due to prolonged sitting. This may lead to discomfort and difficulty concentrating or completing tasks, and over time, it can lead to musculoskeletal disorders like repetitive strain injuries.
Emotional and Psychological Impact
The physical limitations caused by muscle stiffness can take a toll on mental and emotional health. The persistent discomfort and frustration of not being able to perform everyday tasks can lead to various psychological effects.
Decreased Quality of Life
Frustration and Anxiety: Chronic muscle stiffness often leads to a feeling of frustration as individuals may become more dependent on others or feel less capable of managing their own affairs. This can result in feelings of helplessness or anxiety.
Depression: If muscle stiffness and the pain it causes become long-term, individuals may experience depression due to limited mobility, reduced participation in social or recreational activities, and an overall decrease in well-being.
Loss of Independence: In severe cases, muscle stiffness can lead to a loss of independence. For example, difficulties with mobility or self-care may necessitate assistance from others, which can contribute to feelings of isolation and loss of autonomy.
Reduced Social Participation
Social Isolation: Individuals dealing with chronic stiffness may avoid social events or group activities because of discomfort or the fear of being unable to participate fully. This can lead to social isolation, further contributing to depression or anxiety.
Reluctance to Exercise: People with muscle stiffness may be less inclined to engage in physical activities, including group fitness classes, recreational sports, or even walking with friends. This avoidance of exercise can perpetuate the cycle of stiffness and worsen both physical and mental health.
Risk of Injury and Long-Term Consequences
Chronic muscle stiffness, if not addressed, can lead to a higher risk of injury. The tightness in muscles reduces flexibility and balance, making individuals more prone to falls and accidents.
Increased Fall Risk
Balance and Coordination: Stiff muscles, particularly in the legs and lower body, affect an individual’s balance and coordination, increasing the risk of falls, especially in older adults. Muscle tightness can result in slower reactions and less controlled movement, which makes slipping or tripping more likely.
Slower Reflexes: Stiff muscles take longer to contract and extend, which can delay responses to sudden changes in the environment. This delayed reaction time increases the likelihood of falls and injuries.
Medications and Drug Side Effects
- Cause: Some medications can cause muscle stiffness as a side effect. For example, statins (cholesterol-lowering drugs) and certain antipsychotic medications are known to contribute to muscle tightness and rigidity.
- Mechanism: Drugs that affect the nervous system, such as those used to treat psychiatric or neurological conditions, can cause abnormal muscle movements or stiffness as part of their side effects.
- Identification: Muscle stiffness caused by medications is often generalized and can occur along with other side effects such as fatigue, weakness, or tremors.
- Management: If medication is the cause, it may be necessary to adjust the dosage or switch to a different drug. Under the supervision of a healthcare professional, this must be done .
Signs and Symptoms of Muscle Stiffness
Rigidity in Muscles
Description: The most noticeable symptom of muscle stiffness is a sensation of tightness or rigidity in the affected muscles. Muscles may feel tense, making it harder to move them freely.
Common Areas Affected: This feeling of tightness is most commonly experienced in the neck, back, shoulders, arms, legs, and calves. The feeling is frequently stronger in the morning or following extended periods of inactivity.
Tenderness
Description: In addition to stiffness, muscles may also be sore or tender to the touch. The pain may be dull and aching or sharp, especially when the muscle is stretched or moved.
Location: This pain is typically felt in the affected muscle groups, such as the back, neck, legs, or arms, and can be exacerbated by physical activity or overuse.
Swelling or Inflammation
In certain instances, the affected area may experience swelling or inflammation in addition to stiffness. This can occur due to injury, overuse, or underlying conditions like arthritis.
Symptoms: Swelling may be noticeable, and the area may feel warm to the touch or appear red.
Weakness in the Affected Muscles
Description: Muscle stiffness may also be associated with weakness, where the muscles feel fatigued or less capable of performing certain movements. This can make it harder to perform everyday tasks or participate in physical activities.
Impact on Function: Weakness can occur when the stiff muscles are not able to generate enough force or endurance, making it difficult to lift objects, walk, or climb stairs.
Decreased Flexibility
A perceptible reduction in flexibility is one of the most obvious effects of muscular stiffness.The muscles may resist stretching, making it harder to move freely or perform movements that require flexibility.
Common Areas Affected: Stiffness in the back, hamstrings, and shoulders can limit overall mobility and flexibility.
Fatigue or General Discomfort
Description: Muscle stiffness can lead to a general feeling of discomfort and fatigue, particularly in the morning or after physical activity. This can result from muscle overuse, inactivity, or prolonged sitting.
Effects: The discomfort might affect daily activities, making it harder to perform tasks such as walking, exercising, or sitting for extended periods.
Tension Headaches
Tension headaches can be caused by tense muscles, particularly in the neck and shoulders. These headaches are often accompanied by pain and tightness in the scalp, neck, and upper back.
Triggering Factors: Poor posture, stress, or poor sleeping positions can contribute to the development of tension headaches associated with muscle stiffness.
Stiffness that Worsens After Rest
Description: Muscle stiffness is often more pronounced after periods of inactivity, such as after sleeping or sitting for long periods. The muscles may feel particularly stiff and sore upon waking up or standing up after sitting for a long time.
Morning Stiffness: This is a common symptom of muscle stiffness, particularly in people who have been inactive for an extended period.
Diagnosis of Muscle Stiffness
Diagnosing muscle stiffness involves a comprehensive approach, where healthcare providers assess the patient’s medical history, conduct a physical examination, and may use additional diagnostic tools to identify the underlying cause. Muscle stiffness can stem from a variety of factors, including physical exertion, poor posture, neurological disorders, or chronic conditions like arthritis or fibromyalgia. Accurate diagnosis is crucial to determine the best treatment and management strategy for the individual.
Medical History and Symptom Review
The first step in diagnosing muscle stiffness involves a detailed discussion between the patient and the healthcare provider. The provider would inquire regarding the patient’s :
- Onset of Symptoms: When did the stiffness begin? Did it develop suddenly or gradually?
- Location of Stiffness: Which specific muscles or areas of the body are affected? Is the stiffness localized or widespread?
- Duration: How long does the stiffness last? Is it constant or intermittent? Does it improve with rest or worsen after physical activity?
- Associated Symptoms: Are there other symptoms present, such as pain, weakness, swelling, numbness, or difficulty moving? Is there a history of joint pain, headaches, or fatigue?
- Potential Triggers: Were there any specific events or activities that seemed to trigger or worsen the stiffness, such as heavy exercise, an injury, stress, or long periods of inactivity?
- Previous Medical Conditions: The healthcare provider will ask about any history of chronic conditions such as arthritis, fibromyalgia, or neurological disorders (e.g . Parkinson’s disease) that may contribute to muscle stiffness.
- Utilization of Medication: As a side effect, certain drugs may produce muscle tightness or stiffness. Patients will be asked about any medications they are currently taking, including over-the-counter drugs, supplements, and prescribed treatments.
Physical Examination
The physical examination is a critical part of diagnosing muscle stiffness. During this process, the healthcare provider will assess the affected muscles and joints through a series of steps:
- inspection: The doctor will look for visible signs of muscle stiffness, swelling, or bruising. The patient’s range of motion, posture, and gait will also be observed.
- Palpation: The healthcare provider may gently press or palpate (feel) the muscles to assess tenderness, tightness, or the presence of muscle knots or spasms.
- Range of Motion Testing: The provider will ask the patient to move their muscles or joints in different directions to test flexibility and identify any limitations in movement.
- Muscle Strength Testing: The strength of the affected muscles will be tested to see if there is any weakness accompanying the stiffness. The patient is frequently asked to push or pull in opposition to resistance to achieve this.
- Neurological Examination: The doctor may perform a neurological exam to assess muscle reflexes, coordination, and sensory function. This helps to identify any nerve-related causes of stiffness, such as neuropathy or neurological disorders.
laboratory Tests
In some cases, laboratory tests may be necessary to confirm or rule out certain conditions that can cause muscle stiffness. These tests may include:
Blood Tests:
- Creatine Kinase (CK) Levels: Elevated CK levels can indicate muscle damage or inflammation, which may be a sign of conditions such as rhabdomyolysis (muscle breakdown), muscle injury, or inflammatory muscle diseases.
- Thyroid Conditions: In addition to weariness and weight gain, hypothyroidism can result in widespread muscle weakness and stiffness.
- Inflammatory Markers: Blood tests to measure markers like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR) can indicate the presence of inflammation in the body, which may be related to conditions like arthritis or autoimmune disorders.
- Electrolyte Levels: Low levels of electrolytes such as calcium, potassium, and magnesium can contribute to muscle cramps or stiffness, and a blood test can help identify imbalances.
- Urinalysis: A urinalysis may be conducted to assess kidney function, particularly in cases where muscle stiffness is associated with muscle breakdown (rhabdomyolysis), as this condition can lead to kidney damage.
Imaging Studies
Imaging tests can be used to see the bones, joints, and muscles to find any injuries or structural irregularities. These may include:
- X-rays: X-rays may be used to check for joint degeneration, bone fractures, or signs of osteoarthritis, which can contribute to muscle stiffness and discomfort. However, X-rays are not typically useful for diagnosing muscle problems directly.
- MRI (Magnetic Resonance Imaging): An MRI scan can provide detailed images of the muscles, soft tissues, and nerves. It is especially useful for detecting muscle strains, tears, or inflammation, as well as conditions like herniated discs or nerve compression, which may lead to muscle stiffness.
- Ultrasound: An ultrasound can be used to assess soft tissue injuries, such as muscle strains or tears. It is often used to detect swelling or other issues in the muscles and tendons.
Electrodiagnostic Studies
For suspected neurological causes of muscle stiffness (e.g., nerve compression or disorders like multiple sclerosis or Parkinson’s disease), electrodiagnostic tests may be used:
- Electromyography: it conducts the electrical activity in muscles. It can help determine whether muscle stiffness is related to nerve dysfunction or muscle pathology. For instance, it can identify indications of muscular damage or anomalies in muscle activity.
- Studies on Nerve Conduction: These assessments gauge how effectively electrical impulses go through nerves. Nerve-related disorders such as peripheral neuropathy and carpal tunnel syndrome, which can result in muscle rigidity, can be diagnosed with the aid of nerve conduction investigations.
Differential Diagnosis
Muscle stiffness can be caused by a wide range of conditions, so healthcare providers will consider several possible diagnoses to rule out other causes. These may include:
- Muscle Overuse: Stiffness due to physical activity, especially after intense or unfamiliar exercise, is a common cause and is usually temporary.
- Fibromyalgia: A disorder marked by persistent muscle soreness and stiffness, frequently coupled with exhaustion and irregular sleep patterns.
- Arthritis: Osteoarthritis, rheumatoid arthritis, or other inflammatory arthritis conditions can cause muscle stiffness, particularly around the joints.
- Neurological Conditions: Conditions such as Parkinson’s disease, multiple sclerosis, or dystonia can cause muscle stiffness due to impaired nerve function.
- Myopathies: These are diseases that directly affect the muscle tissue, such as inflammatory myopathies (e.g. polymyositis, dermatomyositis) or muscular dystrophy.
- thyroid conditions: hypothyroidism can result in fatigue, weight gain, and widespread muscle weakness and stiffness.
- Medications: Certain medications, such as statins (cholesterol-lowering drugs), can cause muscle stiffness as a side effect.
- Electrolyte Imbalances: Deficiencies in calcium, potassium, or magnesium can lead to muscle cramps or stiffness.
Specialized Tests for Chronic Conditions
For more chronic or complex cases of muscle stiffness, specialized tests may be ordered to investigate long-term or underlying health conditions:
Muscle Biopsy: In rare cases, a muscle biopsy may be performed to examine the muscle tissue for any signs of disease, such as muscular dystrophy, inflammatory myopathy, or other rare conditions.
Genetic Testing: If a hereditary muscle disorder is suspected, genetic testing may be performed to identify mutations associated with muscular dystrophy or other inherited muscle diseases.
Treatments and Remedies for Muscle Stiffness
Conservative treatment
Over-the-Counter Medications: Analgesics and Anti-Inflammatories for Muscle Stiffness
Over-the-counter (OTC) medications are widely available and commonly used to treat muscle stiffness, pain, and inflammation. Analgesics and anti-inflammatory drugs are the two primary groups into which these treatments usually fall. Both types of drugs can help manage muscle stiffness, but they work in different ways to provide relief.
Analgesics: Pain Relievers
Drugs known as analgesics reduce pain without addressing the underlying cause of the discomfort. While they don’t reduce inflammation, they can be very effective in reducing the discomfort associated with muscle stiffness and soreness.
Acetaminophen (Tylenol)
How it works: Acetaminophen is an ordinary analgesic that functions by blocking pain motions in the brain. Although it lacks anti-inflammatory qualities, its main uses are to lower fever and treat mild to moderate discomfort.
When to use: Acetaminophen is effective for treating mild muscle stiffness and pain when inflammation is not a significant concern. It is often used when the stiffness is not associated with swelling or injury.
Dosage: Typically taken every 4-6 hours as needed, with a maximum of 4,000 mg per day to avoid liver damage. If the package contains particular dosage instructions, always read it.
Side effects: Acetaminophen is generally considered safe when taken as directed, but excessive use can cause liver damage. People with liver disease or chronic alcohol use should consult a healthcare provider before using it
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
NSAIDs are medications that relieve pain and reduce inflammation, making them a good choice for treating muscle stiffness that involves inflammation or swelling. They are often preferred when muscle stiffness is caused by overexertion, injury, or conditions like arthritis.
Ibuprofen (Advil, Motrin)
How it works: Ibuprofen is a popular NSAID that works by inhibiting the production of prostaglandins, which are chemicals in the body that promote inflammation, pain, and fever. In order to alleviate pain and edema, ibuprofen lowers prostaglandins.
When to use: Ibuprofen is effective for managing muscle stiffness related to inflammation. It can help reduce swelling and alleviate both acute and chronic muscle pain, such as that caused by muscle strains or arthritis.
Dosage: The typical dosage for adults is 200-400 mg every 4-6 hours, with a maximum daily dose of 1,200 mg. Always take the recommended dosage as directed on the packaging.
Side effects: While ibuprofen is effective for pain relief, it can cause stomach irritation, ulcers, or gastrointestinal bleeding when taken in high doses or for prolonged periods. It may also elevate blood pressure and affect kidney function in some individuals, especially when used long-term.
Naproxen (Aleve)
How it works: Naproxen is another NSAID that works in a similar manner to ibuprofen but has a longer duration of action. It helps reduce pain and inflammation by inhibiting prostaglandin production.
When to use: Naproxen is suitable for individuals who need longer-lasting relief from muscle stiffness and inflammation. It is effective for treating conditions like muscle strains, tendinitis, or arthritis-related muscle pain.
Dosage: Naproxen is typically taken as 220 mg every 8-12 hours, with a maximum of 660 mg per day for over-the-counter use. It is important to adhere to the recommended dosing schedule to avoid complications.
Side effects: Similar to ibuprofen, naproxen can cause gastrointestinal issues such as stomach upset, ulcers, and bleeding. It may also increase the risk of cardiovascular problems when used long-term.
Aspirin (Bayer, Bufferin)
How it works: Aspirin is one of the oldest and most well-known NSAIDs. It works by blocking the enzyme cyclooxygenase (COX), which is responsible for the formation of prostaglandins. This reduces pain, inflammation, and fever.
When to use: Aspirin can be effective for managing mild muscle stiffness and soreness, especially when inflammation is present. It is also used for its blood-thinning properties in cardiovascular health.
Dosage: For pain relief, aspirin is usually taken in doses of 325-650 mg every 4-6 hours, with a maximum daily dose of 4,000 mg.
Side effects: Aspirin can irritate the stomach lining, leading to ulcers, gastrointestinal bleeding, or upset stomach. It should be avoided by individuals with certain conditions like gastrointestinal disorders or those taking blood thinners.
Topical Analgesics and Anti-Inflammatories
In addition to oral medications, topical treatments are available that can be applied directly to the skin to relieve muscle stiffness and pain. These treatments provide localized relief and are often used for muscle soreness, sprains, or strains.
Menthol-Based Creams (Biofreeze, Icy Hot)
How it works: Menthol is a common active ingredient in many topical analgesics. It creates a cooling sensation on the skin, which can help distract from pain and promote blood circulation in the affected area. It also has mild anti-inflammatory properties.
When to use: Menthol-based creams are often used for temporary relief of mild muscle stiffness and soreness. They can be especially helpful for conditions like back pain, neck stiffness, or joint pain.
Dosage: As instructed, apply these lotions to the afflicted area three to four times daily.
Side effects: While generally safe, menthol creams can cause skin irritation in some individuals. They should not be applied to skin that is damaged or inflamed.
Capsaicin Creams (Zostrix, Capzasin)
How it works: Capsaicin is derived from chili peppers and works by depleting the substance P, a neurotransmitter involved in pain signaling. This reduces the pain sensation over time when applied topically.
When to use: Capsaicin creams are effective for chronic muscle stiffness and pain, especially in conditions like arthritis, fibromyalgia, or muscle tightness. After consistent application, capsaicin creams offer long-lasting relief.
Dosage: Three to four times a day, apply a tiny bit of capsaicin cream to the afflicted area. It may take several days of consistent use to feel the full effects.
Side effects: Capsaicin can cause a burning sensation upon initial application, which usually subsides with continued use. Redness or inflammation of the skin can originate from it.
Arnica Creams (Arnicare)
How it works: Arnica is a plant-based product that is used in topical creams to reduce pain and swelling.
When to use: Arnica is particularly effective for relieving muscle stiffness caused by trauma, such as strains or sprains. It is oftentimes devoted to sprains, bruises, and painful muscles.
Dosage: Massage the afflicted area two to three times a day with arnica cream or gel.
Side effects: Arnica is generally safe when used topically, but it should not be applied to broken skin. Allergies or skin irritation may occur in certain people.
Choosing the Right Medication for Muscle Stiffness
When choosing an over-the-counter medication for muscle stiffness, consider the following factors:
Type of pain: If the muscle stiffness is associated with inflammation (e.g., from a sprain or strain), NSAIDs like ibuprofen or naproxen are typically more effective than acetaminophen, as they target both pain and inflammation.
Duration of use: If you need relief for a longer period, naproxen may be preferred over ibuprofen, as it has a longer duration of action.
Pre-existing conditions: If you have a history of gastrointestinal issues (e.g., ulcers), acetaminophen may be a safer choice than NSAIDs. For individuals with heart disease or kidney issues, NSAIDs should be used with caution and under the guidance of a healthcare provider.
Topical vs. oral: Topical treatments may be preferred if you want to avoid the side effects of systemic medications, especially for localized muscle stiffness.
Prescription Treatments: Muscle Relaxants and Other Drugs for Muscle Stiffness
When over-the-counter treatments are not enough to alleviate muscle stiffness or pain, prescription medications may be necessary. Muscle relaxants, along with other prescription drugs, are commonly used to treat more severe cases of muscle stiffness, particularly when it is associated with conditions like muscle spasms, spasticity, or chronic pain disorders.
Muscle Relaxants
Muscle relaxants are a class of drugs designed to relieve muscle spasms and reduce muscle tone. They are often prescribed when muscle stiffness is caused by conditions like acute muscle strains, spinal cord injuries, or neurological disorders such as multiple sclerosis or cerebral palsy.
Cyclobenzaprine (Flexeril)
How it works: Cyclobenzaprine is one of the most commonly prescribed muscle relaxants. It reduces muscle spasms and encourages muscle relaxation by obstructing nerve signals (or pain feelings) that are transmitted to the brain.
When to use: Cyclobenzaprine is typically prescribed for short-term use to treat acute muscle spasms and stiffness caused by injury or overuse. It is not typically used for chronic conditions, as long-term use may lead to side effects.
Dosage: The usual starting dose is 5 mg taken 3 times daily, which can be increased to 10 mg if needed. Usually, a prescription is given for a few days to two weeks.
Side effects: Fatigue, dry mouth, lightheadedness, and sleepiness are typical side effects. More serious side effects, though rare, include heart problems, especially in people with heart disease. It should be avoided in individuals with certain conditions such as hyperthyroidism or glaucoma.
Methocarbamol (Robaxin)
How it works: Methocarbamol is a centrally acting muscle relaxant that works by inhibiting nerve transmission in the brain and spinal cord, which helps relax muscles and reduce spasms. Unlike some other muscle relaxants, it does not have a significant sedative effect.
When to use: Methocarbamol is often prescribed for acute muscle spasms resulting from injury, strains, or overexertion. It may also be used in the treatment of conditions like tetanus, which causes severe muscle rigidity.
Dosage: The typical dosage for muscle spasms is 1,500 mg four times per day during the first 48-72 hours, after which the dose may be reduced. Usually, it is given for short durations of time.
Side effects: Side effects can include drowsiness, dizziness, nausea, and headache. Methocarbamol may also cause allergic reactions, though this is rare. If you experience any unexpected symptoms, it’s crucial to speak with a healthcare professional.
Baclofen (Lioresal)
How it works: Baclofen is a muscle relaxant that works by acting on the central nervous system, specifically the spinal cord, to reduce muscle spasticity and tightness. It is often used for conditions that involve chronic muscle spasms, such as multiple sclerosis, spinal cord injuries, or cerebral palsy.
When to use: Baclofen is prescribed for both acute and chronic muscle stiffness, particularly when it is associated with conditions causing spasticity. It is more commonly used for long-term management than other muscle relaxants.
Dosage: Baclofen is typically started at a low dose, such as 5 mg three times a day, with gradual increases to 20-80 mg per day depending on the patient’s response. It is available in both oral and intrathecal (spinal) forms for severe cases.
Side effects: Typical adverse effects involve weakness, exhaustion, lightheadedness, and sleepiness. It can also cause nausea, confusion, and, in rare cases, liver issues or seizures. Abruptly stopping baclofen can lead to withdrawal symptoms, including increased spasticity and hallucinations, so it should be tapered under a healthcare provider’s supervision.
Tizanidine (Zanaflex)
How it works: Tizanidine is a centrally acting alpha-2 adrenergic agonist that helps relax muscles by blocking nerve signals in the spinal cord. It is particularly effective for managing muscle spasticity and is commonly prescribed for conditions like multiple sclerosis and spinal cord injuries.
When to use: Tizanidine is typically used for managing muscle spasms and spasticity in chronic conditions. It can also be used for acute muscle spasms, but it is most commonly prescribed for long-term management of spasticity.
Dosage: Tizanidine is usually started at 2 mg once a day and can be increased to 4 mg every 6-8 hours, depending on the individual’s response. It should be taken as directed, as excessive doses can lead to sedation or low blood pressure.
Typical adverse effects comprise weakness, exhaustion, lightheadedness, and sleepiness. Rare but serious side effects may include liver damage, so regular liver function tests are recommended during long-term use. Abrupt discontinuation can lead to rebound spasticity and withdrawal symptoms.
Other Prescription Drugs for Muscle Stiffness
In some cases, muscle stiffness may be part of a broader condition, such as fibromyalgia, chronic pain syndrome, or neurological disorders. In these instances, a healthcare provider may prescribe other medications to help manage both the underlying condition and the muscle stiffness.
Anticonvulsants
Anticonvulsant medications, such as Gabapentin and Pregabalin (Lyrica), are often used for neuropathic pain, which can be a source of chronic muscle stiffness and spasms.
How they work: These medications help to calm overactive nerves by reducing nerve signaling in the brain and spinal cord. This is especially useful for treating conditions like fibromyalgia, diabetic neuropathy, and post-herpetic neuralgia, where nerve pain contributes to muscle discomfort.
Dosage: Gabapentin is often started at 100-300 mg per day, gradually increasing to 1,800 mg per day depending on the individual’s response. The usual dosage of pregabalin is 75 mg twice daily, with the possibility of rising to 150–300 mg daily.
Anticonvulsants may cause edema, weight gain, drowsiness, and lightheadedness as side effects. Rare side effects may include mood changes, suicidal thoughts, and allergic reactions.
Antidepressants (Amitriptyline)
Some antidepressants, especially tricyclic antidepressants (TCAs) like Amitriptyline, are used to manage chronic pain, including muscle stiffness and pain associated with fibromyalgia, neuropathy, and other conditions.
How they function: Amitriptyline and related medications reduce pain and enhance sleep by raising the brain’s concentration of neurotransmitters like serotonin and norepinephrine. For those who experience both discomfort and sleep difficulties, this is especially helpful.
Dosage: Amitriptyline is often taken at night. A low starting dose of 10–25 mg is then progressively raised as needed to reach 100 mg per day.
Constipation, tiredness, weight gain, dry mouth, and blurred eyesight are typical adverse effects. It is also important to note that these medications can have sedating effects, and they should not be used in combination with certain other medications due to possible interactions.
Opioids (for Severe Pain)
Opioid medications like Hydrocodone, Oxycodone, and Morphine may be prescribed in cases of severe, chronic pain, including muscle stiffness that does not respond to other treatments. However, opioids are generally not first-line treatments due to their potential for addiction and side effects.
How they function: Opioids block pain signals and provide potent pain relief by attaching to opioid receptors in the brain and spinal cord.
When to use: Opioids are usually prescribed only when other pain management options have failed and the pain is severe. They are not recommended for long-term use due to the risk of dependence, addiction, and overdose.
Side effects: Opioids have a range of side effects, including drowsiness, constipation, nausea, respiratory depression, and risk of addiction. Due to these side effects, opioids should be used with caution and under strict medical supervision.
Choosing the Right Prescription Treatment
The choice of prescription medication for muscle stiffness depends on several factors, including:
- The underlying cause: If the stiffness is related to muscle spasms, muscle relaxants like cyclobenzaprine or methocarbamol may be effective. If the stiffness is due to neurological conditions like multiple sclerosis or spinal cord injuries, drugs like baclofen or tizanidine may be more appropriate.
- Duration of symptoms: For short-term muscle stiffness due to injury, muscle relaxants may be sufficient. For chronic muscle stiffness, anticonvulsants, antidepressants, or other long-term treatments may be needed.
- side effect description: The adverse effects of various drugs vary. For example, some muscle relaxants may cause sedation, while others, like methocarbamol, have fewer sedative effects.
- Other health conditions: If you have a history of liver or kidney issues, cardiovascular problems, or other chronic health conditions, your healthcare provider will choose medications that are safest for you.
Heat and Cold Therapy for Muscle Stiffness
Heat and cold therapies are two of the most widely used and effective home remedies for alleviating muscle stiffness, pain, and inflammation. Both therapies have distinct mechanisms of action and can be used for different types of muscle discomfort. They are non-invasive, cost-effective, and easy to apply, making them accessible options for managing muscle stiffness at home.
Heat Therapy
Heat therapy, also known as thermotherapy, is often used to treat chronic muscle stiffness, soreness, and tightness. By enhancing blood flow to the afflicted area, providing heat to muscles assists in relaxing them and reducing pain. This can be particularly useful for muscle stiffness caused by tension, overuse, or injury.
How Heat Therapy Works: Heat works by increasing the temperature of the tissues, which expands blood vessels, increases circulation, and relaxes muscles. The greater flow of blood helps the muscles eliminate waste products from metabolism, which can cause discomfort and stiffness, while also supplying oxygen and minerals. Heat also reduces the sensation of pain by stimulating sensory receptors in the skin, which can override pain signals sent to the brain.
When to Use Heat Therapy
Heat therapy is generally used for muscle stiffness associated with:
- Tension in the muscles: Caused by worry or stress.
- Chronic pain: Such as back pain, arthritis, or general muscle tightness.
- Post-exercise soreness: For relief from muscle stiffness after physical activity.
- Injuries that are no longer in the acute stage: Once inflammation and swelling have subsided, heat can help with the recovery process by increasing blood circulation and promoting muscle relaxation
Types of Heat Therapy
- Hot Packs: A traditional and simple method involves using hot packs, which can be purchased or made at home. Typical illustrations involve electrically heated pads and steaming water bottles. Heat packs should be applied to the affected area for about 15-20 minutes, ensuring that they are warm but not too hot to avoid burns.
- Warm Towels: Soaking a towel in warm water and applying it to the stiff muscles can provide relief. This method is portable and convenient, especially for areas like the neck, shoulders, and back.
- Heating Pads: Electric heating pads or microwavable gel pads are excellent tools for delivering consistent heat to larger areas like the back or thighs.
- Warm Baths: Soaking in a warm bath, especially one with Epsom salts, can relax muscles and reduce stiffness. Further relief is provided by the water’s buoyancy, which also relieves joint pressure.
Benefits of Heat Therapy
- Muscle relaxation: Heat helps relax tense muscles, which is beneficial for conditions like muscle cramps or spasms.
- Improved circulation: The increase in blood flow promotes healing in damaged tissues and helps reduce pain.
- Pain relief: Heat can relieve pain by reducing the muscle’s response to stress and tension.
- Enhanced flexibility: By increasing the flexibility of muscles and joints, heat therapy can aid in improving the range of motion.
Precautions When Using Heat Therapy
- Avoid use during acute inflammation: Heat should not be applied immediately after an injury that involves swelling or inflammation (such as a sprain or strain) because it can worsen the swelling. In these situations, cold treatment is more suitable.
- Monitor skin sensitivity: Always use a layer of cloth or towel between your skin and the heat source to avoid burns. Stay away from heat for longer than twenty to thirty minutes at a time to prevent overheating or skin damage.
- Avoid if you have certain medical conditions: People with conditions like diabetes or poor circulation should consult with a healthcare provider before using heat therapy, as it can affect blood flow.
Cold Therapy
Cold therapy, also known as cryotherapy, is used primarily to reduce inflammation, swelling, and pain associated with acute muscle injuries, sprains, strains, or conditions that cause inflammation. It slows blood flow and lessens swelling and inflammation by tingling the afflicted area and narrowing blood vessels.
How Cold Therapy Works: Cold therapy reduces blood flow to the affected area by restricting blood vessels, a process known as blood vessel constriction. This helps to minimize inflammation and swelling, as well as numb the area to reduce pain. By cooling the tissues, cold therapy also helps slow the nerve transmission of pain signals, providing temporary relief.
When to Use Cold Therapy
The best results from cold therapy come right after an injury, like:
- Acute muscle injuries: Sprains, strains, and tears.
- Inflammation: Conditions such as tendinitis or bursitis that cause swelling and discomfort.
- Swelling: To reduce swelling in joints or muscles after an injury.
- Post-surgical recovery: To control swelling after surgery.
- Exercise-induced soreness: It can help reduce muscle soreness if applied soon after intense physical activity.
Types of Cold Therapy
- Ice Packs: Putting an ice pack wrapped in a towel or piece of cloth on the afflicted area is the most popular method of cold therapy. Between therapeutic treatments, the skin can warm up by using cold packs for between fifteen and twenty minutes at a time.
- Ice Massage: This involves using a block of ice to massage the affected area. This method can be particularly useful for smaller areas, like the neck or shoulders.
- Cold Compresses: You can use cold compresses, which are available as gel packs that can be refrigerated or frozen, to provide consistent cold therapy to larger muscle areas.
- Frozen Vegetables: In the absence of a commercial ice pack, a bag of frozen peas or corn can serve as an effective and flexible cold pack.Cold Baths: For more extensive areas of muscle stiffness, a cold bath or ice bath (where you submerge the body part or your entire body in ice-cold water) may be beneficial. This is common after intense physical activity or in the treatment of certain sports injuries.
Benefits of Cold Therapy
- Reduction in inflammation: Cold therapy helps decrease swelling and inflammation caused by injuries or overuse.
- Pain relief: The numbing effect of cold reduces pain and discomfort, making it easier to manage muscle stiffness.
- Prevention of muscle spasms: Cold can help prevent muscle spasms by reducing muscle activity and preventing the inflammatory process.
- Faster recovery: Cold therapy can speed up recovery time after intense physical activity or injuries by reducing muscle damage and swelling.
Precautions When Using Cold Therapy
Steer clear of lengthy use: Cold therapy shouldn’t be used concurrently for longer than twenty minutes. Prolonged exposure to cold can lead to frostbite or nerve damage.
Applying ice or cold packs immediately to the skin should never be done because this might cause harm to the skin. Instead, cover them in a towel or cloth.
Do not use on areas with poor circulation: People with conditions like Raynaud’s disease or poor circulation should avoid using cold therapy on affected areas.
Avoid the presence of infection: Cold therapy may exacerbate certain infections by reducing blood flow to the area, so it should not be used if there is a known infection in the muscle or joint.
Combining Heat and Cold Therapy
In some cases, alternating between heat and cold therapies can provide enhanced relief for muscle stiffness. This method is called contrast therapy, and it combines the benefits of both heat and cold to promote healing and reduce discomfort.
How it works: Cold therapy reduces inflammation and numbs the area, while heat therapy increases circulation and promotes muscle relaxation. Alternating between the two therapies can help break the cycle of pain and stiffness, providing both immediate relief and long-term healing benefits.
When to use: Contrast therapy is especially useful for chronic conditions, like back pain or muscle tension, where inflammation and stiffness are persistent. It can also be used after exercise to reduce muscle soreness and stiffness.
How to do it: One method involves applying cold therapy for 5-10 minutes, followed by heat therapy for 15-20 minutes, and then repeating the process. Always finish with cold therapy if you are using it for an injury, as this helps to control swelling.
Physical Therapy for Muscle Stiffness
Physical therapy is a highly effective treatment for muscle stiffness, offering targeted, evidence-based interventions to address both the symptoms and underlying causes. This form of treatment not only helps alleviate discomfort but also aims to restore normal muscle function, improve flexibility, strengthen weak muscles, and prevent future occurrences of stiffness.
Physical therapy’s function in alleviating muscle stiffness
Physical therapy (PT) is designed to improve physical function through a series of therapeutic exercises, manual techniques, education, and modalities. When addressing muscle stiffness, PT helps the body recover by improving mobility, restoring muscle length and function, and reducing pain. Here’s how physical therapy is specifically beneficial for muscle stiffness:
Restoring Range of Motion (ROM): One of the key goals of PT is to restore joint mobility and flexibility. Physical therapists use a variety of manual techniques (e.g., joint mobilizations, soft tissue massage) and exercises to improve the range of motion of stiff muscles and affected joints. These interventions can help increase the flexibility of the muscle fibers and the joint structures, which improves movement and reduces stiffness.
Strengthening Muscles: Muscle stiffness is often linked to muscle weakness or imbalances, especially when muscles are not being activated properly. Physical therapists develop personalized strengthening programs to target weak muscles, improve stability, and balance muscle function. Strengthening exercises help relieve stiffness by making muscles more resistant to strain, preventing them from tightening up under stress.
Improving Posture and Body Alignment: Poor posture is one of the leading causes of muscle stiffness, especially in the neck, shoulders, back, and hips. Physical therapists assess posture and teach patients exercises that improve body alignment, strengthen the core, and balance the muscles around key joints. Correcting posture reduces the risk of stiffness by ensuring that muscles work in their optimal positions during daily activities.
Relieving Pain: Physical therapists use various modalities to reduce pain associated with muscle stiffness. These can include heat or cold therapy, ultrasound, electrical stimulation (e.g., TENS units), and manual therapy techniques like massage or trigger point therapy. By managing pain, physical therapy allows patients to engage more effectively in movement and exercise, further promoting recovery and mobility.
Facilitating Recovery After Injury: Muscle stiffness is often a consequence of injury, whether acute (e.g., muscle strains) or chronic (e.g., tendonitis or arthritis). PT is an essential part of recovery from musculoskeletal injuries. Therapists help patients regain function and prevent complications such as muscle atrophy, scar tissue formation, or joint stiffness by incorporating targeted exercises and manual therapy into the treatment plan.
Preventing Recurrence: A major benefit of physical therapy for muscle stiffness is its emphasis on prevention. To prevent future muscular tension, physical therapists teach their patients about ergonomics, stretching methods, and appropriate body mechanics. Additionally, PT can improve strength and flexibility, making muscles less prone to overuse injuries and tightness.
Developing a physical therapy plan for muscle stiffness
When developing a physical therapy treatment plan for muscle stiffness, a therapist will perform a comprehensive assessment to determine the cause, severity, and location of the stiffness. Based on this evaluation, the therapist will create a personalized treatment program that addresses the underlying factors contributing to the stiffness and helps improve mobility. A typical physical therapy plan for muscle stiffness might include:
- Initial Evaluation: The therapist will conduct a thorough assessment, including a physical examination and possibly imaging studies (if needed), to assess muscle function, joint movement, posture, and pain levels.
- Goal Setting: The therapist and patient will set specific, measurable goals for treatment, such as improving range of motion, decreasing pain, or increasing muscle strength.
- Treatment Plan: Based on the evaluation, the therapist will develop a treatment plan that may include a combination of manual therapy, therapeutic exercises, modalities, posture education, and other techniques.
- Progress Tracking: Throughout the therapy process, the therapist will track progress, adjust the plan as needed, and re-evaluate the patient’s function to ensure that the therapy is effective.
Techniques used in physical therapy for muscle stiffness
Physical therapy employs a variety of techniques, each designed to address specific aspects of muscle stiffness. Here are some of the most commonly used PT methods to treat muscle stiffness:
Mechanical therapy
Electrical Stimulation (E-Stim)
Applying a small electrical current to the skin is known as electrical stimulation, and it includes transcutaneous electrical nerve stimulation (TENS). This current stimulates the nerves and helps reduce pain, muscle spasms, and inflammation. E-stim can also promote muscle relaxation and improve circulation to stiff muscles.
How Electrical Stimulation Works: Electrical Stimulation (E-Stim) works by applying a controlled electrical current to specific areas of the body. Electrodes are applied to the skin close to the injured muscle or nerve to administer the current. Depending on the settings, the electrical current can stimulate nerve fibers to block pain signals, promote muscle contraction, or increase blood flow to the targeted area.
There are several types of E-Stim, each designed for specific purposes:
Transcutaneous Electrical Nerve Stimulation (TENS):
Purpose: TENS is primarily used for pain relief and muscle relaxation.
How it works: TENS uses low-frequency electrical currents to stimulate the sensory nerves, blocking pain signals from reaching the brain and promoting the release of endorphins, the body’s natural painkillers.
Application for Muscle Stiffness: TENS can be used to alleviate pain and discomfort associated with muscle stiffness, particularly for conditions like fibromyalgia, chronic muscle tightness, and acute muscle strains.
Neuromuscular Electrical Stimulation (NMES):
Purpose: NMES is used to stimulate muscle contractions and improve muscle function.
How it works: NMES uses a stronger electrical current than TENS to activate motor nerves, causing the muscle to contract. This contraction mimics natural muscle activity and can help improve muscle strength, reduce atrophy, and reduce stiffness in the targeted area
Application for Muscle Stiffness: NMES is often used in rehabilitation to stimulate weak or inactive muscles, improve circulation, and reduce muscle stiffness caused by injury or disuse.
Interferential Current Therapy (IFC):
IFC is extensively utilized to treat pain and reduce inflammation.
How it works: IFC involves the use of two medium-frequency currents that intersect at the area of pain or muscle stiffness, creating a deeper electrical stimulation that is more comfortable for the patient.
Application for Muscle Stiffness: IFC is effective in treating deep muscle pain, muscle tightness, and stiffness by improving blood flow, reducing inflammation, and relieving pain.
Functional Electrical Stimulation (FES):
Purpose: FES is used to help patients with impaired motor function regain normal movement.
How it works: FES delivers electrical pulses to specific muscles to generate muscle contractions, helping to restore movement patterns in individuals with nerve damage or conditions like stroke, spinal cord injury, or multiple sclerosis.
Application for Muscle Stiffness: FES can assist with muscle activation and reduce stiffness in cases where muscle function has been impaired due to neurological conditions or immobilization.
Applications of electrical stimulation for muscle stiffness
Electrical Stimulation can be applied in various settings, from home use with portable units to clinical treatments under the guidance of a trained healthcare professional. The specific application depends on the type of muscle stiffness and its underlying cause. Below are common scenarios where E-Stim is applied to treat muscle stiffness:
- Post-Injury or Post-Surgery Recovery: After an injury or surgery, muscle stiffness is a common issue. E-Stim can help reduce swelling, improve circulation, and relax muscles that have become tight or stiff due to disuse. It also helps maintain muscle strength and function during the recovery phase.
- Chronic Muscle Conditions (e.g., Fibromyalgia, Chronic Pain): Conditions such as fibromyalgia or chronic muscle pain can cause persistent muscle stiffness. E-Stim, particularly TENS, is commonly used to provide long-term relief from muscle pain and stiffness associated with these conditions.
- Sports Injuries and Overuse: Athletes often experience muscle stiffness due to overuse or excessive training. E-Stim helps ease tense muscles, lessen discomfort, and hasten the healing process after sprains, strains, or overuse ailments like tendinitis.
- Post-Exercise Muscle Soreness (DOMS): Delayed-onset muscle soreness (DOMS) is common after intense physical activity. E-Stim can help alleviate the stiffness and soreness that occurs 24 to 48 hours after exercise by promoting blood flow and reducing muscle tension.
- Neurological Conditions: Conditions like stroke, multiple sclerosis, and spinal cord injury can impair muscle function and cause stiffness due to poor nerve signaling. Functional Electrical Stimulation (FES) is used to improve muscle activation, reduce stiffness, and restore normal movement patterns in such cases.
- Rehabilitation and Prehabilitation: In rehabilitation programs, E-Stim can be used to treat muscle stiffness caused by immobilization or disuse. It can also be used as part of rehabilitation programs to strengthen muscles before surgery, reducing the risk of stiffness and muscle weakness afterward.
Precautions and Considerations for E-Stim
While E-Stim is a safe and effective treatment for muscle stiffness in most individuals, there are a few precautions and considerations to keep in mind:
Not Suitable for Everyone: E-Stim should not be used by individuals with certain medical conditions, such as pacemakers, implanted defibrillators, or electrical implants, as the electrical impulses can interfere with the functioning of these devices. It should also be avoided in individuals with certain heart conditions, epilepsy, or skin infections.
Proper Electrode Placement: Correct placement of the electrodes is crucial for the effectiveness of E-Stim. Improper placement can result in discomfort or reduced efficacy. A trained healthcare professional should guide electrode placement, especially during the initial treatments.
Avoid Use on the Head or Neck (without supervision): E-Stim should generally not be used on the head or neck areas without professional supervision due to the risk of adverse effects, particularly near the carotid artery or sensitive nerve areas.
Duration of Treatment: The duration and intensity of E-Stim treatments should be carefully controlled to avoid overstimulation of the muscles. Treatments that are too long or too intense can lead to muscle fatigue or discomfort
Manual Therapy
Manual therapy refers to hands-on techniques that physical therapists use to manipulate muscles, joints, and connective tissues to reduce stiffness, pain, and tension. Some manual therapy techniques include:
Joint Mobilization
Joint mobilization is a technique that involves the therapist using controlled, passive movements to improve the range of motion (ROM) of stiff or restricted joints. This technique can be applied to areas such as the spine, hips, shoulders, and knees. The goal of joint mobilization is to relieve pain, improve mobility, and reduce muscle stiffness that results from joint dysfunction or tightness.
Techniques Used:
Grade I Mobilization: Low-velocity movements designed to relieve pain and reduce joint stiffness by moving the joint within its normal range.
Grade II Mobilization: Slightly higher intensity movements that help increase ROM and decrease joint tightness.
High-velocity motions that lengthen the joint capsule and expand ROM mobility are known as grade III mobilization.
Grade IV Mobilization: The most intense form of mobilization, used to stretch the joint capsule and improve mobility in cases of severe stiffness.
Myofascial Release
The fascia, the connective tissue that envelops muscles, bones, and joints, is the focus of a technique known as myofascial release.. This method relieves stiffness, increases flexibility, and lessens discomfort by providing constant pressure to particular fascial sites of tension. Fascia can become stiff or restricted due to injury, overuse, or poor posture, which may contribute to muscle stiffness.
Techniques Used:
Direct Myofascial Release: The therapist applies sustained pressure to the tight areas of the fascia using their hands, fingers, or elbows. Restoring regular movement patterns and relieving tension are the objectives.
Indirect Myofascial Release: The therapist applies gentle, controlled pressure in the direction of the restriction, helping to stretch and release the fascia.
Benefits of Myofascial Release:
- Reduces muscle and fascia stiffness
- accelerate the motion and muscular flexibility
- Alleviates pain caused by fascial tightness
- bring back limited parts’ natural range of motion and functionality
Muscle Energy Techniques (MET)
Muscle energy techniques are a form of manual therapy that involves the patient actively engaging their muscles while the therapist applies resistance. The patient contracts their muscles against the therapist’s resistance, followed by a relaxation phase, which helps stretch and lengthen the muscles. MET is particularly useful for muscle stiffness and tightness caused by muscle imbalances or chronic tension.
Techniques Used:
Isometric Contraction: The patient contracts a muscle without changing its length, holding the contraction for a few seconds before relaxing. This lessens stiffness and boosts muscle flexibility.
Isotonic Contraction: The patient contracts the muscle and holds the position while the therapist provides gentle resistance. This technique helps to stretch the muscles and promote relaxation.
Benefits of Muscle Energy Techniques:
- Reduces muscle stiffness and tightness
- boost muscle flexibility and ROM
- Restores muscle balance and reduces muscle imbalances
- furnish ease from muscle spasms and tension
Craniosacral Therapy (CST)
A soft, manual method, craniosacral treatment concentrates on the motion of the fluid and membranes that surround the brain and spinal cord. It is primarily used to release tension in the soft tissues of the head, neck, and spine, but it can also help alleviate muscle stiffness throughout the body. CST aims to balance the craniosacral rhythm and improve the functioning of the nervous system, which can help reduce muscle stiffness and pain.
Techniques Used:
Gentle Touch: The therapist applies light pressure to the head, neck, and spine to detect any imbalances or restrictions in the craniosacral system.
Releasing Tension: The therapist gently releases any areas of tension or restriction by applying soft, rhythmic pressure to promote relaxation and balance.
Benefits of Craniosacral Therapy:
- Reduces tension and stiffness in the head, neck, and spine
- enhance the nerve system’s performance
- Alleviates chronic pain and muscle stiffness
- Promotes deep relaxation and stress relief
Therapeutic Exercise
Therapeutic exercises are a cornerstone of physical therapy, and they help address muscle stiffness by improving strength, flexibility, and mobility. Usually customized to meet the individual needs of the patient, these exercises could consist of:
Stretching: Static, dynamic, and PNF stretching are among the methods used to extend tense muscles. The goal is to gradually improve flexibility and muscle length to reduce stiffness.
Strengthening Exercises: Focused on building strength in muscles that are weak, which can contribute to poor posture and stiffness. Strengthening exercises often target the core, lower back, and other key muscle groups to provide support and reduce strain on stiff areas.
Range of Motion Exercises: These exercises assist in regaining mobility in muscles and joints that are stiff. They focus on controlled movement through the full range of motion to reduce tightness and prevent joint stiffness.
Stretching for muscle stiffness
Stretching and physical therapy are essential tools in the management and prevention of muscle stiffness. Regular stretching and targeted physical therapy exercises help maintain muscle flexibility, increase range of motion, alleviate pain, and promote overall muscle function. Both approaches are integral to rehabilitation following injury, managing chronic conditions, and enhancing overall mobility and performance.
Stretching Techniques for Muscle Stiffness
Stretching is a key component of any fitness or rehabilitation routine. It is especially beneficial for people experiencing muscle stiffness, as it helps to lengthen tight muscles, improve flexibility, and prevent further injury. The secret to increasing flexibility and avoiding stiffness is consistency.
Static Stretching
How Static Stretching Works: Static stretching works by gently elongating the muscles and connective tissues. The goal is to increase muscle flexibility and range of motion by gradually stretching the muscle fibers and fascia (the connective tissue that surrounds muscles). By holding the stretch, the muscle is given time to lengthen, which can alleviate tightness and improve flexibility over time. When a stretch is held for an extended period, the muscle spindle (the sensory receptor that detects changes in muscle length) adapts to the stretch, leading to a reduction in muscle tension and a more relaxed state. Static stretching is often performed after exercise as part of a cool-down routine, but it can also be beneficial on its own for alleviating muscle stiffness.
How It Helps Muscle Stiffness: Static stretches can improve the flexibility of stiff muscles by gently increasing their length. It helps to reduce tightness, increase blood flow, and improve the range of motion in the affected area.
How to Perform Static Stretching
To maximize the benefits of static stretching, it is essential to follow the correct technique and approach. Here is a step-by-step guide on how to perform static stretches:
Warm Up: Spend five to ten minutes engaging in a light cardiovascular activity, such as walking, jogging, or cycling, to warm up your muscles before completing static stretches. This ready the muscles for stretching by increasing blood flow to them.
Choose a Stretch: Select the appropriate stretch for the muscle or muscle group that feels stiff. Focus on one stretch at a time and avoid overstretching.
Stretch Slowly: Move into the stretch slowly and gently, avoiding any jerky or bouncing movements. The stretch should be comfortable and should not cause sharp pain. Stretch the muscle until you notice a slight tug or strain.
Maintain the Stretch: After you’ve achieved a comfortable stretch, maintain it for 15 to 30 seconds. Let your muscles progressively lengthen by taking a deep breath and letting yourself relax into the stretch. Do not bounce or use quick movements, as this can increase the risk of injury.
Repeat: Repeat the stretch 2-4 times for each muscle group, depending on your flexibility goals and the level of stiffness you’re experiencing.
Common static stretches for muscle stiffness
Here are some common static stretches that target key muscle groups, helping to relieve stiffness and improve flexibility:
Hamstring Stretch
How to Perform: The sole of your foot should rest against the inner thigh of the leg you are extending, so sit on the floor with one leg bent and put the other leg directly in front of you. With both hands, reach forward toward the extended leg’s toes. Have the stretch for 15 to 20 seconds, sensing a rhythmic stretch along the back of the leg.
Repeat with the other leg.
Quadriceps Stretch
How to Perform: For balance, cling to a chair or wall while standing up.
Pull your heel toward your buttocks by bending one knee behind you and using your hand to grab the ankle or foot.
Keep your knees together and hips squared forward. Hold for 20-30 seconds.
Repeat with the other leg.
Shoulder Stretch
How to Perform: When standing or sitting, keep your back straight.
Lengthen one arm across the body and extend it in front of the wall.
Use the opposite arm to gently pull the extended arm closer to your chest, feeling a stretch in the shoulder.
Repeat on the opposite side after containing for 15 to 20 seconds.
Calf Stretch
How to Perform: Place your hands against a wall while facing it.
Step back one foot while maintaining a straight back leg and both feet flat on the ground.
Maintaining the back heel on the floor, lean forward into the wall till the calf of the back leg starts to stretch.
I’ve to fifteen seconds of holding, then repeat on the other leg.
Chest Stretch
How to Perform: preserve the feet shoulder-width apart and stand tall.
arrange the hands behind the back and lengthen the arms.
Stretch your chest by opening your shoulders and removing your hands from your body as you slowly raise your arms upward.
preserve chest stretch for 10 to 15 seconds.
Precautions when performing static stretching
While static stretching is generally safe, it is important to follow these precautions to avoid injury and maximize the benefits:
- Avoid Bouncing: Do not bounce or jerk during static stretching, as this can lead to muscle strain. Always move into the stretch rhythmically and grasp it.
- Do Not Stretch to Pain: Stretching should never be painful. Stop right away if you experience sudden, intense discomfort during stretching. Stretching should cause mild discomfort, but not intense pain.
- Don’t Overstretch: It’s important to avoid overstretching the muscles. Stretching too far can cause muscle strain or ligament damage. Aim for a comfortable stretch, and gradually increase the stretch over time.
- Be Consistent: For lasting flexibility and relief from muscle stiffness, it’s important to stretch regularly. The secret to increasing flexibility and avoiding stiffness is consistency.
- Breath Deeply: Remember to breathe deeply and steadily while holding the stretch. Holding your breath can create additional tension in your muscles and reduce the effectiveness of the stretch.
Dynamic Stretching
Dynamic stretching is a type of stretching that uses fluid, coordinated motions to extend the muscles and joints to their maximum potential. Unlike static stretching, which requires holding a stretch for some time, dynamic stretching is more active and often performed as part of a warm-up before physical activity or exercise. It is designed to prepare your muscles and joints for movement, enhance flexibility, and reduce the risk of injury.
How to Perform Dynamic Stretching
To perform dynamic stretching effectively, it’s important to focus on smooth, controlled movements rather than rushing through the stretches. Below are guidelines for performing dynamic stretches properly:
Start with a Warm-Up: Before starting dynamic stretches, do a light aerobic warm-up such as jogging, brisk walking, or cycling for 5–10 minutes to get the blood flowing and to raise your body temperature.
Focus on the Movement: Each dynamic stretch should involve controlled, smooth movements. To prevent yourself from getting hurt, avoid jerky or fast motions.
Work Within a Comfortable Range of Motion: You should move to the point where you feel a slight stretch or resistance in the muscles but not pain. Gradually increase the intensity and range of motion as your body becomes more accustomed to the movement.
Perform Each Stretch for 30–60 Seconds: Each dynamic movement should be done for a certain number of repetitions, generally between 8 and 15 for each side of the body. Take it slow and perform each stretch with control.
Focus on Specific Muscle Groups: Target the muscle groups that will be used most in your workout or sport. If you’re preparing for a run, for example, focus on stretches for the hamstrings, hip flexors, and calves.
How It Helps Muscle Stiffness: Dynamic stretching helps to activate and warm up the muscles, which is particularly useful for reducing stiffness before physical activity. It also helps to improve coordination and flexibility in muscles and joints.
Common Dynamic Stretches for Muscle Stiffness
Here are some effective dynamic stretches that can help relieve muscle stiffness and prepare your body for physical activity:
Leg Swings
How to Perform: For balance, place yourself near a wall or other stable object.
progressively extend the range of motion by carefully swinging one leg forth and backward.
Perform 10-15 swings for each leg.
Benefits: Leg swings are great for loosening up the hip flexors, hamstrings, and glutes. They also help increase flexibility in the lower body.
Arm Circles
How to Perform: maintain an erect pose with your feet shoulder-width apart and your arms extended out to the sides.
Make small circles with your arms, gradually making them larger as you go.
execute 15-20 circles in each path (clockwise and counterclockwise).
Benefits: This exercise warms up the shoulders, improves shoulder joint mobility, and releases tension in the upper body.
Lunge with a Twist
How to Perform: With your right leg, take a step forward into the position of a lunge, making sure your knee and ankle line up.
As you lunge, twist your torso toward the right leg, reaching your left hand toward the outside of your right knee.
move back to the initial pose and repeat with the left leg.
Perform 5-10 repetitions per side.
Benefits: This stretch activates the hip flexors, quads, hamstrings, and core while also increasing flexibility in the spine.
High Knees
How to Perform: Stand tall and march in place, bringing each knee up to your chest one at a time as high as possible.
Keep a brisk pace, aiming for 30-45 seconds of high knees.
Benefits: High knees are excellent for increasing circulation, warming up the hip flexors, quadriceps, and calves, and helping to reduce muscle stiffness in the lower body.
Walking Lunges
How to Perform: preserve a straight posture and place your feet shoulder-width apart.
Take a step forward with one leg and lower your body into a lunge position, making sure your knee is at a 90-degree angle.
Push off the back leg to bring it forward and perform a lunge on the opposite leg.
Continue lunging forward for 10-12 repetitions on each side.
Benefits: Walking lunges target the glutes, quads, hamstrings, and calves, helping to reduce stiffness while enhancing flexibility and joint mobility.
Toy Soldiers (Straight-Leg Kicks)
How to Perform: Stand tall and extend your arms in front of you.
Kick one leg straight up while keeping it as straight as possible, aiming to touch your foot to your hand.
Repeat ten to fifteen times on every side, switching legs.
Benefits: Toy soldiers are an excellent dynamic stretch for hamstrings, hip flexors, and lower back flexibility.
Hip Circles
How to Perform: Position both hands on the hips and your feet hip-width away.
gradually move the hips in a circular motion, generating large circles.
Perform 10-15 rotations clockwise, then switch to counterclockwise.
Benefits: This movement helps release stiffness in the hip joints and lower back, making it a great warm-up for activities that require leg movement.
When to Use Dynamic Stretching
Before Exercise: Dynamic stretching is most beneficial as part of your warm-up routine before engaging in physical activity, sports, or exercise. It activates muscles, increases flexibility, and prepares your body for movement.
To Relieve Muscle Stiffness: If you’re experiencing stiffness due to sitting for long periods, physical labor, or after a workout, dynamic stretching can help release tightness and improve mobility.
As a Regular Flexibility Routine: Dynamic stretches can also be incorporated into a regular flexibility routine to improve range of motion, flexibility, and overall muscle health.
.Precautions with Dynamic Stretching
While dynamic stretching is generally safe, it’s important to follow these precautions:
Start Slow: Begin with gentle movements and gradually increase the intensity and range of motion as your body becomes accustomed to the movements.
Avoid Jerky Movements: Keep all motions controlled and smooth to avoid straining muscles or joints.
pay attention to your body: Take note of your body’s sensations while performing the stretches. If you feel any discomfort or pain, stop immediately and consult a healthcare provider or physical therapist.
PNF (Proprioceptive Neuromuscular Facilitation) Stretching
Proprioceptive Neuromuscular Facilitation (PNF) stretching is a highly effective and advanced form of stretching used to enhance flexibility and range of motion. Initially developed as a rehabilitation technique for patients with neuromuscular disorders, PNF is now widely used by athletes and individuals seeking to improve muscle flexibility, relieve stiffness, and improve overall muscle performance.
PNF stretching combines both passive stretching and isometric contraction (contracting a muscle without changing its length) to increase the length of muscles and improve flexibility. This technique is typically performed with a partner or trainer, but some variations can be done alone.
How PNF Stretching Works
PNF works by taking advantage of the body’s natural neurological response to muscle contractions and relaxation. The key mechanisms involved in PNF stretching include:
Stretching (Initial Lengthening): The muscle to be stretched is initially lengthened in a controlled manner, usually through passive stretching, to put it in a stretched position.
Isometric Contraction: After the muscle has been stretched, the individual then contracts the muscle isometrically against resistance (typically from a partner) for a short period (usually 5–10 seconds). This action activates the muscle’s proprioceptors—specifically the Golgi tendon organs (GTO), which are responsible for monitoring muscle tension.
Relaxation: After the isometric contraction, the muscle is allowed to relax briefly (usually 10–20 seconds) before it is stretched again. During this relaxation phase, the muscle becomes more pliable, and the range of motion increases.
Repeat the Stretch: This process is typically repeated 2–3 times for each muscle group to achieve the best results.
How It Helps Muscle Stiffness: PNF stretching involves a combination of muscle contraction and relaxation, which enhances muscle lengthening and reduces stiffness. It is particularly effective in overcoming muscle tightness and increasing flexibility.
Techniques of PNF Stretching
Several variations of PNF stretching are commonly used, including the Hold-Relax, Contract-Relax, and Hold-Relax-Contract methods. Each method involves slightly different processes but generally follows the same principles of stretching, isometric contraction, and relaxation.
Hold-Relax Technique
Step 1: The muscle is passively stretched to the point of mild discomfort.
Step 2: The individual then contracts the stretched muscle isometrically against the partner’s resistance for 5-10 seconds. The contraction should be strong, but not painful.
Step 3: After the isometric contraction, the muscle is relaxed for about 10–20 seconds.
Step 4: The muscle is then stretched again to a deeper position than before, and the process is repeated.
This method is one of the simplest and most commonly used forms of PNF stretching.
Contract-Relax Technique
Step 1: The muscle is passively stretched to its end range.
Step 2: The individual then contracts the muscle concentrically (actively shortening the muscle) against resistance from the partner for 5-10 seconds.
Step 3: After the contraction, the muscle is relaxed for 10–20 seconds.
Step 4: The muscle is then stretched again, typically achieving a greater range of motion than the first stretch.
The contract-relax technique emphasizes concentric muscle contraction (shortening of the muscle), which allows for a greater stretch when the muscle is relaxed.
Hold-Relax-Contract Technique
Step 1: The muscle is passively stretched to the point of mild discomfort.
Step 2: The individual contracts the muscle isometrically against resistance for 5-10 seconds.
Step 3: The muscle is then relaxed for a short period (10-20 seconds).
Step 4: The muscle is then actively contracted concentrically (shortened) against resistance for 5-10 seconds.
Step 5: After the concentric contraction, the muscle is stretched again, achieving the deepest stretch.
The hold-relax-contract method combines both isometric and concentric contractions, and it is often used to achieve the greatest possible increase in range of motion.
How to Perform PNF Stretching
Although PNF stretching can be performed with a partner, it is possible to modify some of these techniques to be done alone, although having assistance is ideal for maximizing the benefits.
Here is a basic guide to performing PNF stretching:
- Warm-Up: Always perform a light aerobic warm-up for 5–10 minutes before doing PNF stretching. This prepares the muscles and joints for deeper stretching.
- Partner or Equipment Setup: If working with a partner, have them provide resistance during the isometric contraction. If stretching alone, use equipment like a resistance band or towel to simulate the partner’s resistance.
- Positioning: Start by passively stretching the target muscle to a comfortable stretch, not pushing into pain. This initial stretch should be held for a few seconds.
- Contract the Muscle: Next, contract the muscle for 5-10 seconds against resistance. Be sure the contraction is controlled and strong, but not to the point of pain.
- Relaxation Phase: After the contraction, allow the muscle to relax for about 10–20 seconds. This is where the muscle becomes more pliable.
- Re-stretch: Now, stretch the muscle again, trying to achieve a deeper stretch than before.
- Repeat: Perform this sequence for 2–3 rounds for each muscle group. It’s important to keep the movements controlled and gradual, avoiding jerking or sudden movements.
Precautions with PNF Stretching
While PNF stretching is highly effective, it requires caution due to its intensity and involvement of isometric contractions. Here are some important precautions:
- Warm Up Properly: PNF stretching should never be done without a proper warm-up. Cold muscles might get injured when stretched.
- Avoid Overstretching: Do not push into pain during the stretching phase. PNF is effective for improving flexibility, but overstretching can lead to muscle strain or injury.
- Control the Contraction: The isometric contraction should be strong but not forced. It should be done in a controlled manner to prevent muscle strain.
- Work with a Qualified Partner: Ideally, PNF stretching should be done with a knowledgeable partner who can provide adequate resistance and ensure proper technique. Improper resistance can lead to injury.
- Avoid If Injured: If you have an injury, particularly in the muscle or joint being stretched, PNF stretching should be avoided until you have consulted with a healthcare professional.
When to use PNF Stretching
For Improving Flexibility: PNF is an excellent method for increasing flexibility, especially when targeting specific muscles that are tight or stiff.
In Rehabilitation: Due to its effectiveness in improving muscle flexibility and range of motion, PNF stretching is commonly used in physical therapy and rehabilitation after injuries.
For Athletes: Athletes who require high levels of flexibility or mobility in their sport often incorporate PNF stretching into their routine to enhance muscle performance and prevent injuries.
Active Stretching
Active stretching is a form of flexibility exercise that involves holding a stretch using the strength of the muscles without the assistance of an external force such as a partner, wall, or gravity. In active stretching, you stretch a muscle by actively contracting the muscle that is opposite to the one being stretched, allowing you to hold the stretch for a period of time. Active stretching is typically performed dynamically, with controlled movements, and it’s particularly effective in enhancing flexibility, strength, and endurance.
How active stretching works: Active stretching works by using the strength of the opposing muscle group (known as the antagonist) to stretch the target muscle (the agonist). This type of stretch relies solely on the muscles being used to hold the position, without assistance from external forces.
Examples of Active Stretches
Here are some common active stretching exercises that target different muscle groups:
Leg Raises (Hip Flexors & Hamstrings)
How to Perform: Lie on your back with one leg extended on the floor and the other leg bent.
Slowly raise the extended leg, keeping it straight, until it is parallel to the floor.
Hold the raised position using the strength of your quadriceps, while stretching the hamstring on the opposite leg.
Hold for 10–20 seconds, then lower the leg and switch sides.
Muscle Focus: Hamstrings, hip flexors.
Active Butterfly Stretch (Groin and Inner Thighs)
How to Perform: Place the feet together and bend your legs out to the sides while you sit.
Use your leg muscles to gently press your knees toward the floor while keeping your back straight.
Engage your inner thighs as you try to stretch your groin.
Hold for 15–20 seconds.
Muscle Focus: Groin, inner thighs.
Shoulder and Arm Swings (Shoulders and Upper Body)
How to execute: Stand with your feet shoulder-width separated.
Extend your arms out in front of you and swing them open wide, then bring them back together in front of your chest.
Repeat this motion in a controlled manner, increasing the range of motion as you go.
Perform for 30–60 seconds.
Muscle Focus: Shoulders, chest, and upper back.
Active Hamstring Stretch (Hamstrings)
How to conduct: Stand straight and lift one leg straight in front of you, preserving the knee straight.
While keeping the lifted leg extended, flex your foot to engage your hamstrings.
Hold this position for 10–15 seconds and switch legs.
Muscle Focus: Hamstrings.
Active Quadriceps Stretch (Quadriceps)
How to Perform: Stand tall and bend one knee, bringing your foot toward your glutes.
Contract your quadriceps to hold the stretch, using the strength of your opposing leg to stabilize the position.
preserve for 10–20 seconds, then transit sides.
Muscle Focus: Quadriceps.
Massage therapy and its effectiveness for muscle stiffness
Massage therapy is a widely recognized treatment for muscle stiffness, soreness, and tension. It involves the manipulation of soft tissues, such as muscles, tendons, and ligaments, using various techniques to promote relaxation, improve circulation, and relieve discomfort. Whether used to alleviate acute muscle stiffness, chronic pain, or post-exercise soreness, massage therapy can be a highly effective tool in managing muscle stiffness and enhancing overall well-being.
How Massage Therapy Works
Massage therapy works by applying pressure, friction, and movement to the body’s soft tissues. The primary mechanisms through which massage therapy helps relieve muscle stiffness include:
- Increased Blood Flow: When pressure is applied to the muscles, it helps improve circulation. Increased blood flow helps the muscles receive oxygen and nutrients while also eliminating waste products from metabolism, including lactic acid, which can cause stiffness and pain. This process accelerates healing and reduces muscle tightness.
- Release of Tension: Massaging muscles helps to break up adhesions or knots (also known as myofascial trigger points) that form in the muscle tissue, which can contribute to pain and stiffness. These knots can be the result of poor posture, stress, or overuse, and releasing them can bring significant relief.
- Stimulation of the Nervous System: The gentle pressure of massage stimulates the parasympathetic nervous system, which is responsible for promoting relaxation. This can help reduce the body’s stress response, lower cortisol levels, and alleviate muscle tension caused by anxiety or stress. Improved Flexibility: Regular massage therapy can help increase the flexibility of muscles and connective tissues, which can be beneficial for individuals dealing with chronic stiffness or those recovering from injuries. Stretching the muscles during massage helps restore their natural elasticity and range of motion.
Types of Massage Techniques for Muscle Stiffness
Several types of massage therapy techniques can be used to treat muscle stiffness, each offering distinct benefits. Among the most popular methods are:
Swedish Massage
Swedish massage is one of the most popular forms of therapeutic massage and is typically used for general relaxation and muscle stiffness. It involves long, flowing strokes, kneading, and rotary motions on the outer layers of muscles.
Effectiveness for Muscle Stiffness: Swedish massage promotes relaxation by calming the nervous system and increasing circulation to the muscles, which can help relieve tension and discomfort. It is ideal for individuals who are experiencing mild to moderate muscle stiffness, particularly from tension or stress.
Deep Tissue Massage
Deep tissue massage targets the deepest levels of muscle tissue and fascia (the connective tissue that surrounds muscles) by applying gradual, firm pressure. This technique is especially effective for chronic muscle stiffness and tightness that has persisted for a longer period.
Effectiveness for Muscle Stiffness: By working deeper into the muscles, deep tissue massage helps break up scar tissue, release muscle knots, and alleviate chronic tension. This technique is particularly beneficial for people suffering from conditions like back pain, fibromyalgia, or repetitive strain injuries.
Trigger Point Therapy
Certain “trigger points” or regions of tense, uncomfortable muscles that can radiate pain to other body parts are the focus of trigger point therapy. These points are frequently brought on by stress, injury, or misuse of the muscles. In this technique, sustained pressure is applied directly to the trigger points to relieve muscle tension and reduce referred pain.
Effectiveness for Muscle Stiffness: Trigger point therapy is effective for addressing localized muscle stiffness and pain caused by muscle knots or tight bands of muscle. It helps release the tension in these specific areas and can provide long-lasting relief from discomfort.
Sports Massage
Sports massage is designed for athletes or active individuals who experience muscle stiffness from exercise, sports, or physical activity. It incorporates techniques from Swedish, deep tissue, and trigger point massage to target areas of tightness, enhance flexibility, and reduce recovery time after intense physical activity.
Effectiveness for Muscle Stiffness: Sports massage can help alleviate post-workout muscle stiffness, improve range of motion, and reduce the risk of injury. It is beneficial both before and after exercise to prepare muscles for activity and to aid in recovery.
Effectiveness of Massage Therapy for Specific Conditions
Massage therapy is effective in managing muscle stiffness associated with a variety of conditions, including:
- Fibromyalgia: A condition characterized by widespread muscle pain and stiffness, fibromyalgia can benefit from massage therapy. Studies have shown that regular massage can reduce pain, improve sleep quality, and enhance overall well-being in individuals with fibromyalgia.
- Chronic Back Pain: Chronic back pain, often caused by muscle stiffness, poor posture, or injury, can be alleviated with massage therapy. Research suggests that deep tissue and myofascial release techniques are particularly effective for treating lower back stiffness and pain.
- Tension Headaches: Tension headaches, which are often caused by tightness in the neck, shoulders, and upper back, can be relieved with massage therapy. Massage can lessen the frequency and severity of headaches by focusing on these regions.
- Sports Injuries: Athletes and active individuals often experience muscle stiffness due to overuse or injury. Sports massage, with its combination of deep tissue techniques and stretching, is effective for managing muscle soreness, stiffness, and post-exercise recovery.
Considerations and Limitations
While massage therapy can be highly effective in relieving muscle stiffness, it is important to keep the following considerations in mind:
Professional vs. Self-Massage: Professional massage therapists have the training and expertise to apply the right techniques and pressure to target areas of stiffness effectively. While self-massage with tools such as foam rollers or handheld massagers can be helpful, it may not provide the same level of relief or precision as a professional treatment.
Not a Cure-All: Massage therapy is most effective when used in conjunction with other treatments, such as stretching, exercise, proper posture, and ergonomic adjustments. It is not a substitute for medical treatment in cases of severe injury or conditions like herniated discs, fractures, or infections.
Potential for Discomfort: In some cases, massage therapy, particularly deep tissue or trigger point therapy, can cause temporary discomfort or soreness. This ought to go away in a few hours to a day. However, if pain persists or worsens after a massage, it is important to consult a healthcare provider.
Postural Training and Ergonomic Education
Physical therapists assess how a patient moves and may provide advice on improving posture and body mechanics. Correcting improper posture or modifying the patient’s environment (e.g., adjusting their workstation) can help alleviate muscle stiffness. This often involves educating the patient on how to sit, stand, and move in ways that reduce strain on muscles.
Postural training involves learning how to position the body in a way that minimizes stress on the muscles, joints, and spine. Proper posture reduces the likelihood of muscle stiffness, discomfort, and injury by maintaining natural spinal curves and preventing the overuse or strain of certain muscle groups. In postural training, individuals are taught how to sit, stand, walk, and sleep in ways that optimize alignment and reduce muscle strain.
Key Principles of Postural Training:
Neutral Spine Alignment: The spine has natural curves in the neck (cervical), upper back (thoracic), lower back (lumbar), and sacral regions. Proper posture involves maintaining these curves without exaggerated forward or backward bending. Keeping the spine in neutral alignment prevents muscle tension and stress on the discs and joints.
Even Distribution of Weight: Proper posture ensures that weight is evenly distributed across the body, reducing the load on any particular muscle or joint. This is crucial when standing, walking, or sitting for extended periods.
Avoiding Slouching or Hunching: Slouching, hunching, or leaning forward puts strain on the neck, shoulders, and lower back muscles, contributing to stiffness. Postural training emphasizes keeping the shoulders back, and chest open, and the head aligned with the spine.
Core Engagement: Strengthening and engaging the core muscles (the muscles of the abdomen, lower back, and pelvis) is essential for supporting the spine and preventing muscle stiffness. Proper postural training includes exercises that promote core strength and stability.
Awareness of Body Position: One of the key goals of postural training is to increase body awareness. By becoming more aware of body positioning throughout the day, individuals can make conscious adjustments to avoid straining muscles and joints
What is Ergonomic Education?
Ergonomics refers to the science of designing and arranging the workspace, tools, and tasks to fit the individual’s needs and capabilities. Ergonomic education focuses on teaching individuals how to adapt to their environment to prevent muscle stiffness, strain, and injury. By making small adjustments to posture, equipment, and work habits, individuals can reduce stress on their muscles and joints, improving comfort and productivity.
Ergonomics applies to various settings, including workplaces, homes, and leisure environments. For instance, ergonomic education is crucial for office workers who spend long hours sitting at desks or for people who perform repetitive tasks, such as assembly line workers, data entry operators, or healthcare professionals.
Key Elements of Ergonomic Education:
Workplace Setup:
Ergonomic education teaches individuals how to set up their workspace to maintain neutral body positions. This includes adjusting chair height, monitor position, keyboard and mouse placement, and desk layout.
Chair and Seat Adjustments:
A proper chair is critical for maintaining good posture. Ergonomic education emphasizes choosing a chair that supports the lower back and encourages a neutral sitting position. It also includes tips on how to adjust the seat height, backrest, and armrests to support the body’s alignment.
Keyboard and Mouse Positioning:
When typing or using a mouse, it’s important to keep the arms at a 90-degree angle to reduce strain on the shoulders, arms, and wrists. Ergonomic education teaches individuals how to place their keyboard and mouse at a height that promotes natural arm positioning.
Standing and Walking Posture:
For those who stand for extended periods, ergonomic education includes tips for proper standing posture, such as distributing weight evenly on both feet, keeping the knees slightly bent, and avoiding leaning forward or slouching.
Task Variation:
Repeating the same motion for long periods can lead to muscle stiffness and overuse injuries. Ergonomic education encourages individuals to vary tasks, take frequent breaks, and change positions throughout the day to reduce the strain on muscles and joints.
Combining Postural Training and Ergonomics
For optimal results in preventing and alleviating muscle stiffness, postural training and ergonomic education should be used together. Here’s how combining the two can benefit an individual:
For optimal results in preventing and alleviating muscle stiffness, postural training and ergonomic education should be used together. Here’s how combining the two can benefit an individual:
Integrated Approach to Alignment: Postural training provides the individual with the knowledge of how to align the body correctly during various activities. Ergonomic education helps adapt the environment (workstations, furniture, tools) to support these postural principles, reducing strain on the muscles.
Behavioral Awareness and Habit Formation: Postural training helps individuals become more aware of their posture throughout the day, while ergonomic education promotes healthy work habits and task management. Together, they create a holistic approach to reducing muscle stiffness and preventing further strain.
Long-Term Prevention: By incorporating both postural training and ergonomic principles into daily life, individuals can create sustainable practices that reduce muscle stiffness over the long term, improving overall health and preventing future discomfort.
Posture correction and Ergonomics in Preventing Muscle Stiffness
Posture correction and ergonomics play a critical role in preventing muscle stiffness, discomfort, and long-term musculoskeletal issues. Poor posture, often exacerbated by improper ergonomics, can contribute to muscle tension, discomfort, and even chronic pain. By understanding the importance of good posture and ergonomic practices, individuals can take proactive steps to minimize the risk of developing muscle stiffness and other related problems
How poor posture contributes to muscle stiffness:
- Muscle Imbalances: Poor posture often leads to uneven distribution of weight and force on the muscles, causing some muscles to become overstretched and weak, while others become tight and overworked. This imbalance can result in stiffness and discomfort.
- Increased Muscle Tension: Bad posture, such as slouching or forward head posture, places unnecessary strain on muscles, especially those in the back, neck, shoulders, and hips. This strain can cause muscles to tighten and become stiff.
- Joint Misalignment: Incorrect posture can misalign the spine and joints, leading to abnormal movement patterns. This misalignment places additional stress on the muscles and ligaments, contributing to muscle stiffness and pain.
- Reduced Flexibility: Prolonged poor posture can limit the range of motion in certain joints, making it harder to stretch or move freely, which in turn can lead to muscle stiffness.
Examples of common postural problems that cause muscle stiffness:
- Forward Head Posture: Often seen in individuals who spend extended periods looking at screens, this posture places strain on the neck, shoulders, and upper back, leading to stiffness and discomfort.
- Rounded Shoulders: Common among people who hunch forward while sitting or standing, this posture can lead to tightness in the chest muscles and weakness in the upper back, causing stiffness and pain.
- Anterior Pelvic Tilt: This occurs when the pelvis tilts forward, often due to prolonged sitting or lack of core strength. It can cause stiffness and pain in the lower back and hips.
How good posture prevents muscle stiffness:
Maintaining good posture helps to distribute the body’s weight evenly across the muscles, reducing the strain placed on any one area. Proper alignment ensures that muscles can function efficiently without unnecessary tension, which in turn reduces the risk of stiffness and discomfort. Key benefits of good posture include:
Better Muscle Function: Proper posture ensures that muscles work in a balanced and coordinated way, reducing the risk of fatigue and stiffness.
Improved Circulation: Good posture allows for better blood flow, which helps deliver nutrients to the muscles and removes metabolic waste products. This lessens muscular discomfort and encourages a quicker recovery.
Decreased Muscle Tension: By aligning the body properly, good posture reduces muscle overuse and the buildup of tension, preventing stiffness and discomfort.
The Role of ergonomics in muscle recovery and prevention of stiffness
Ergonomics is the study of how the body interacts with its environment, particularly in the workplace and home settings. Ergonomics involves designing workspaces and tools that promote optimal posture and reduce strain on the body. Poor ergonomics such as sitting at a desk for long periods without proper support or using poorly designed equipment can lead to muscle stiffness, pain, and long-term injuries.
How ergonomics affects muscle stiffness:
- Sitting for Long Periods: Sitting for extended periods, especially in poor posture, can lead to tightness and stiffness in the lower back, hips, and shoulders. When the spine is not properly supported, muscles in the back and core are forced to work harder to maintain posture, leading to discomfort and fatigue.
- Repetitive Movements: Tasks that require repetitive movements, such as typing, lifting, or twisting, can lead to muscle strain and stiffness. Over time, these repetitive actions can cause muscles to become fatigued, tight, and overworked.
- Incorrect Desk and Chair Setup: Using desks and chairs that are too high, too low, or poorly designed can contribute to bad posture and strain the muscles in the back, neck, and shoulders, resulting in stiffness and discomfort.
Proper ergonomics can prevent muscle stiffness:
Ergonomics focuses on modifying the environment to fit the natural needs of the body, allowing muscles to function without unnecessary strain. By improving the setup of workspaces, home environments, and daily routines, individuals can reduce the risk of muscle stiffness and discomfort. Key ergonomic practices that help prevent stiffness include:
- Proper Chair Height and Support: Ensure your chair is at the correct height so that your feet are flat on the floor and your knees are at a 90-degree angle. A chair with good lumbar support will help maintain the natural curve of your spine and reduce strain on the lower back.
- Keyboard and Monitor Positioning: Your monitor should be at eye level, and your keyboard should be at a height where your elbows remain at a 90-degree angle. This helps prevent forward head posture, rounded shoulders, and wrist strain.
- Standing Desk Options: Alternating between sitting and standing throughout the day can help reduce muscle stiffness caused by prolonged sitting. Standing desks or adjustable desks can encourage more movement and improve posture.
- Footrest and Support: Using a footrest can help maintain proper posture when sitting, particularly if your feet don’t reach the floor. This prevents slouching or leaning forward, which can contribute to muscle stiffness.
Use ergonomic tools and equipment
Invest in ergonomic tools, such as adjustable chairs, desks, or computer accessories, to ensure that your work environment supports good posture. Some additional tools include:
Ergonomic Mouse and Keyboard: These devices are designed to reduce wrist strain and encourage better hand positioning.
Standing Desk or Desk Converter: Alternating between sitting and standing can help reduce muscle stiffness and prevent the negative effects of prolonged sitting.
Alternative Therapies for Muscle Stiffness
Acupuncture for muscle stiffness
Acupuncture is an ancient Chinese therapy that involves inserting thin, sterile needles into specific points on the body to stimulate energy flow and promote healing. It has been used for thousands of years to treat various conditions, including pain, muscle stiffness, and tension.
How acupuncture works: Based on the idea that Qi (pronounced “chee”) represents the body’s life force or vital energy, acupuncture was developed. According to Traditional Chinese Medicine (TCM), Qi flows through the body along specific pathways called meridians. When Qi is blocked or imbalanced, it can lead to pain and discomfort, including muscle stiffness.
The goal of acupuncture is to restore the flow of Qi, balance energy, and promote self-healing. By inserting needles into specific acupuncture points, practitioners believe they can stimulate the body’s natural pain-relieving mechanisms, improve blood circulation, and relax tight muscles.
Acupuncture Techniques for Muscle Stiffness:
- Trigger Point Acupuncture: Involves inserting needles directly into areas of muscle tightness or trigger points (areas of muscle tension). This technique aims to release muscle knots and alleviate pain and stiffness.
- Electroacupuncture: Involves applying a mild electrical current to the needles, enhancing the stimulation of the acupuncture points. This method can help improve blood flow and muscle relaxation.
- Cupping Therapy: Often used alongside acupuncture, cupping involves placing glass or silicone cups on the skin to create a vacuum. This therapy is believed to increase blood flow, relieve muscle stiffness, and promote healing.
Benefits of Acupuncture for Muscle Stiffness:
Pain Relief: Acupuncture stimulates the release of endorphins, the body’s natural painkillers, reducing pain and muscle discomfort.
Improved Blood Circulation: The insertion of needles can enhance blood flow to the affected areas, promoting muscle recovery and reducing stiffness.
Muscle Relaxation: Acupuncture helps to relax tight muscles, which is essential for relieving stiffness and improving flexibility.
Reduced Inflammation: Acupuncture has been shown to reduce inflammation in muscles and joints, providing relief from chronic stiffness caused by inflammatory conditions.
Stress Reduction: Acupuncture can help lower stress and anxiety levels, which may contribute to muscle tightness and tension.
Who can benefit from acupuncture?
Acupuncture is suitable for individuals with various musculoskeletal issues, including:
- Chronic muscle stiffness
- Myofascial pain syndrome
- Fibromyalgia
- Post-injury stiffness
- Stress-induced muscle tightness
Chiropractic Care for muscle stiffness
The diagnosis and treatment of musculoskeletal conditions, especially those involving the spine and joints, are the main goals of chiropractic care. Chiropractors use hands-on techniques to adjust the spine and other joints, aiming to restore proper alignment, improve mobility, and reduce pain and stiffness.
How Chiropractic Care Works:
Chiropractors believe that misalignments or dysfunctions in the spine, known as vertebral subluxations, can interfere with nerve function and lead to pain, stiffness, and other health issues. The goal of chiropractic care is to restore spinal alignment and improve the function of the nervous system, promoting natural healing and muscle relaxation.
Chiropractic techniques for muscle stiffness:
- Spinal Adjustments: Chiropractic adjustments involve applying controlled, manual force to specific joints of the spine or limbs to improve alignment and restore mobility. These adjustments may help alleviate muscle stiffness by improving joint movement and reducing tension in surrounding muscles.
- Soft Tissue Therapy: Chiropractors may use soft tissue techniques, such as massage, stretching, or myofascial release, to target tight muscles and release muscle knots contributing to stiffness.
- Postural Correction: Chiropractors assess posture and alignment to identify areas where muscle stiffness may be caused by poor posture or abnormal movement patterns. Postural adjustments and exercises are often recommended to improve body alignment and prevent stiffness from recurring.
- Heat and Cold Therapy: Chiropractors may also recommend heat or cold therapy to reduce muscle inflammation, increase blood flow, and relax tight muscles.
Who can benefit from chiropractic care?
Chiropractic adjustments may be helpful for people who are :
- Chronic muscle stiffness in the neck, back, or limbs
- Muscle stiffness due to poor posture
- Stiffness caused by herniated discs or spinal misalignments
- Postural imbalances or movement dysfunctions
- Acute or chronic musculoskeletal pain
Aromatherapy for muscle stiffness
Aromatherapy is a therapeutic practice that uses essential oils extracted from plants to improve physical, emotional, and mental well-being. In the case of muscle stiffness, aromatherapy can be used to relax tight muscles, reduce pain, and promote overall relaxation.
How Aromatherapy works: Aromatherapy works by inhaling essential oils or applying them topically to the skin. The scent of essential oils triggers the limbic system, which is the part of the brain responsible for emotions, stress response, and memory. The inherent anti-inflammatory, analgesic (pain-relieving), and muscle-relaxing qualities of several essential oils can aid in the relief of stiff muscles.
Aromatherapy techniques for muscle stiffness:
- Topical Application: Essential oils can be diluted with a carrier oil (such as coconut or jojoba oil) and massaged into stiff muscles. Popular essential oils for muscle stiffness include peppermint, eucalyptus, lavender, and ginger. These oils help soothe muscle tension, reduce pain, and improve circulation.
- Aromatic Inhalation: Inhaling the scent of essential oils can help promote relaxation and reduce stress, which is often a contributor to muscle tension and stiffness. Oils such as lavender, chamomile, and rosemary can be used in a diffuser to create a calming atmosphere.
- Bath Soaks: Adding a few drops of essential oils to a warm bath can help relax stiff muscles and provide relief from tension. Epsom salts can be added to the bath for additional muscle relaxation benefits.
- Compresses: Essential oils can be used in hot or cold compresses to target localized muscle stiffness. For instance, lavender and eucalyptus oils can be added to a warm compress to help relax muscles, while peppermint oil can be used in a cold compress to reduce inflammation.
Benefits of aromatherapy for muscle stiffness:
- Muscle Relaxation: Essential oils like peppermint, wintergreen, and marjoram have natural muscle-relaxing properties that can help release tightness and alleviate stiffness.
- discomfort Relief: Anti-inflammatory and analgesic chemicals found in essential oils like lavender, ginger, and turmeric might lessen discomfort brought on by stiff muscles.
- Stress Reduction: Aromatherapy helps reduce stress and anxiety, which are often associated with muscle tightness. Calming oils like lavender and chamomile can promote relaxation and reduce muscle tension caused by stress.
- Improved Circulation: Some essential oils can help reduce muscle stiffness because of their inherent analgesic (pain-relieving), anti-inflammatory, and muscle-relaxing qualities.
- Convenience and Accessibility: Aromatherapy can be easily incorporated into daily routines, whether through the use of essential oil diffusers, topical applications, or bath soaks.
Who can benefit from aromatherapy?
Aromatherapy can benefit individuals experiencing:
- Chronic muscle stiffness and pain
- Stress-related muscle tension
- Post-exercise or post-injury muscle tightness
- General relaxation and well-being
Cupping Therapy
Cupping therapy is a traditional healing technique that involves placing glass or plastic cups on the skin to create suction. The suction helps to pull up the skin and underlying tissue, increasing circulation and promoting healing.
How cupping helps with muscle stiffness:
- Increases Blood Flow: Cupping increases local blood circulation, which can promote the healing of stiff muscles and relieve tension.
- Relieves Pain: By stimulating the tissues, cupping helps release tight muscles and reduce pain.
- Improves Flexibility: The suction and pressure from the cups help loosen tight muscle fibers, improving flexibility and range of motion.
How It Works:
Cups are placed on the skin, typically on areas with muscle stiffness, and left in place for several minutes.
The suction creates a vacuum that draws the skin upwards, increasing circulation and relieving tightness.
Cupping can be done as a stand-alone treatment or in combination with other therapies like acupuncture or massage.
Biofeedback
Biofeedback is a technique that teaches individuals to control physiological processes such as muscle tension, heart rate, and respiration. By using sensors to measure body functions, individuals can learn to consciously alter their responses to stress and muscle tension.
How biofeedback helps with muscle stiffness:
Increases Awareness: Biofeedback allows individuals to become aware of tension in their muscles, helping them to consciously relax them before stiffness sets in.
Promotes Muscle Relaxation: Through real-time monitoring, biofeedback can teach you how to relax certain muscle groups, reducing overall stiffness and tension.
Stress Management: By learning to control stress responses, biofeedback can reduce the chronic tension that contributes to muscle stiffness.
How It Works:
Sensors are placed on the skin to monitor muscle activity, heart rate, or skin temperature.
The therapist provides feedback based on the data, teaching the individual how to control their body’s stress responses.
Over time, individuals learn to relax muscles on their own and manage stress more effectively.
Hydrotherapy
Hydrotherapy, or water therapy, involves using water to relieve pain and improve physical functioning. The buoyancy and resistance of water can provide a unique environment for muscle relaxation and rehabilitation.
How hydrotherapy helps with muscle stiffness:
- Buoyancy Relief: The buoyancy of water helps reduce the weight and strain placed on muscles and joints, allowing for movement without excess pressure.
- Heat and Cold Therapy: Warm water can soothe and relax stiff muscles, while cold water can help reduce inflammation and numb pain.
- Gentle Movement: Water provides resistance to movement, allowing for gentle exercise that can stretch and strengthen muscles without aggravating stiffness.
How It Works:
- Warm Water Soaks: Soaking in a warm bath or hot tub can help relax tense muscles, promote blood circulation, and reduce pain.
- Cold Compresses: Applying cold compresses or alternating between hot and cold water baths can help manage inflammation and muscle stiffness.
- Water Aerobics: Water exercises in a pool can improve flexibility and strength, easing muscle tension while reducing the impact on the body.
Reflexology
Reflexology is a therapy that involves applying pressure to specific areas on the feet, hands, and ears that correspond to different organs and systems of the body. By stimulating these reflex points, reflexology aims to improve circulation, reduce stress, and promote healing.
How Reflexology Helps with Muscle Stiffness:
Improves Circulation: Reflexology promotes blood flow to areas affected by muscle stiffness, aiding in recovery and reducing tightness.
Reduces Stress: By targeting reflex points, reflexology helps alleviate stress and tension that can contribute to muscle stiffness.
Relieves Pain: Reflexology may help activate the body’s natural pain relief mechanisms, reducing discomfort in stiff muscles.
How It Works:
A reflexologist applies pressure to specific points on the feet, hands, or ears that correspond to areas of tension in the body.
Sessions typically last 30-60 minutes, during which the practitioner works on various reflex zones.
Reflexology can be performed regularly as part of a broader wellness routine to manage and prevent muscle stiffness.
Herbal Remedies
Herbal remedies have been used for centuries to treat various physical ailments, including muscle stiffness. Certain herbs have anti-inflammatory and muscle-relaxing properties that can help relieve muscle tension.
Herbs for Muscle Stiffness:
Turmeric: Contains curcumin, which has potent anti-inflammatory properties that can help reduce muscle pain and stiffness.
Ginger: Known for its anti-inflammatory effects, ginger can help alleviate pain and muscle stiffness. It may be consumed as a tea or applied topically in oil form.
Arnica: Commonly used in topical form, arnica helps reduce inflammation, bruising, and pain. It’s often used in gels, creams, or oils for muscle soreness.
Valerian Root: Valerian is known for its calming and muscle-relaxing effects. It can be taken as a supplement or tea to promote relaxation and reduce muscle stiffness.
How It Works:
Topical Application: Arnica creams or oils can be applied directly to areas of muscle stiffness to reduce inflammation and relieve discomfort.
Herbal Teas: Drink ginger or turmeric tea to reduce internal inflammation and ease muscle pain.
Supplements: Herbal supplements, such as valerian root, may help promote muscle relaxation and improve sleep, allowing for better recovery.
The Role of muscle recovery in preventing stiffness
Muscle recovery plays a crucial role in preventing and alleviating muscle stiffness. When muscles are subjected to intense physical activity or stress, they undergo microscopic damage. This natural process requires a period of rest and rehabilitation to allow muscles to repair, rebuild, and become stronger. Without adequate recovery, muscles may become tight, sore, and stiff, which can impede movement and contribute to discomfort.
The importance of muscle recovery in preventing stiffness
Muscle recovery prevents stiffness by addressing several physiological processes that are impacted by exercise. These processes include:
- Repairing Micro-tears: Intense exercise causes microscopic tears in muscle fibers. These tears need time to heal properly. If muscles do not get adequate time to repair, they can become tight and stiff, leading to discomfort or even more serious injuries.
- Replenishing Energy Stores: During physical exertion, muscles use glycogen as a primary energy source. Post-exercise recovery helps restore glycogen levels, which aids in muscle function and prevents fatigue and stiffness in future workouts.
- Reducing Inflammation: Exercise induces inflammation as part of the natural repair process. While mild inflammation is normal, excessive or persistent inflammation can lead to muscle stiffness and soreness. Proper recovery can help control and reduce this inflammation, allowing for greater flexibility and mobility.
- Promoting Circulation: Recovery strategies like gentle movement and stretching can improve blood flow to the muscles, aiding in nutrient delivery to the healing tissue and removing waste products that contribute to stiffness.
Hydration and Nutrition
Adequate hydration and nutrition are fundamental to muscle recovery. Water plays a key role in maintaining muscle function, reducing cramping, and aiding in the transport of nutrients to muscle cells.
Hydration: muscles are largely composed of water, so staying hydrated is crucial for muscle recovery. stiffness and cramping in the muscles can result from dehydration. Drinking water throughout the day, and electrolytes during long periods of intense physical activity, can ensure muscles are hydrated and functioning optimally.
The Role of hydration in muscle recovery
Hydration is a critical component of muscle recovery, as water makes up a significant portion of muscle tissue and is involved in many physiological processes that contribute to muscle function and repair. Adequate hydration supports the body’s ability to transport nutrients to cells, remove waste products, and maintain fluid balance during and after exercise.
How hydration affects muscle recovery:
Prevents Dehydration and Muscle Fatigue: Dehydration can lead to muscle fatigue, cramps, and impaired performance. When you’re dehydrated, the muscles can’t function optimally, leading to stiffness, weakness, and reduced endurance. By staying hydrated, you ensure that your muscles have the water they need to perform at their best and recover more quickly.
Aids in Nutrient Transport: Water helps transport essential nutrients, such as glucose, amino acids, and electrolytes, to muscle cells. These nutrients are necessary for energy production, muscle repair, and overall recovery. Without sufficient water, nutrient delivery to the muscles is compromised, slowing down the recovery process.
Regulates Electrolyte Balance: Electrolytes such as sodium, potassium, and magnesium play a key role in muscle contraction and nerve function. Hydration is essential for maintaining the balance of these electrolytes, and a lack of fluids can lead to muscle cramps, weakness, and spasms.
Reduces Inflammation and Swelling: Proper hydration helps regulate the body’s inflammatory response after intense exercise. When the body is hydrated, it can more effectively manage the release of inflammatory markers and reduce swelling in the muscles, which can otherwise contribute to pain and stiffness.
Signs of dehydration:
During exercise and recovery, it’s important to monitor your hydration levels. Signs of dehydration include:
- Dark yellow urine
- Dry mouth and throat
- Fatigue or dizziness
- Muscle cramps
- Headache
- Decreased performance
Hydration strategies for muscle recovery:
To optimize muscle recovery, it’s important to stay hydrated throughout the day, not just during exercise. Here are some hydration strategies:
- Drink Water Regularly: Aim to drink water throughout the day, especially before, during, and after exercise. A general guideline is to consume 16-20 ounces of water 2-3 hours before exercise and another 8-10 ounces every 10-20 minutes during exercise.
- Replace Lost Fluids with Electrolytes: After intense exercise, especially in hot and humid conditions, drinking water with added electrolytes can help restore the balance of fluids and prevent muscle cramps. Electrolyte-rich drinks (e.g., coconut water, sports drinks) can help replenish lost sodium, potassium, and magnesium.
- Hydrate Post-Workout: After a workout, focus on rehydrating to help the body recover from fluid loss. Drinking water or an electrolyte solution post-workout can help restore lost fluids, reduce muscle soreness, and improve recovery.
- Monitor Urine Color: A simple way to track hydration status is by observing the color of your urine. Clear to light yellow urine typically indicates proper hydration, while dark yellow or amber-colored urine suggests dehydration.
Nutrition: Proper nutrition supports muscle repair and reduces the risk of stiffness. Protein is essential for muscle tissue repair, while carbohydrates replenish glycogen stores. Healthy fats, vitamins, and minerals (like magnesium and potassium) also contribute to muscle function. Anti-inflammatory foods, such as turmeric, ginger, and fatty fish, can help reduce muscle soreness and inflammation.
Key nutrients for muscle recovery:
Protein: Protein is essential for muscle repair and growth, as it provides the amino acids required to rebuild muscle fibers that have been broken down during exercise. Consuming adequate protein after a workout accelerates muscle repair, reduces muscle soreness, and promotes muscle growth.
How Protein Aids Recovery:
- Muscle Protein Synthesis: Exercise causes muscle fibers to break down, and protein is needed to rebuild and repair these fibers. Protein consumption after exercise enhances muscle protein synthesis (the process of building new muscle proteins), which is essential for recovery.
- Preventing Muscle Breakdown: Protein intake helps prevent muscle breakdown during recovery. After exercise, the body can enter a catabolic (muscle-wasting) state, and protein helps reverse this by supporting anabolic (muscle-building) processes.
- Sources of Protein: Among the best sources of protein are: Lean meats (chicken, turkey, lean beef), Fish (salmon, tuna), Dairy products (Greek yogurt, cottage cheese), Eggs, Plant-based sources (tofu, tempeh, lentils, beans, quinoa )
Carbohydrates:
Carbohydrates are the body’s primary energy source, and they play a key role in muscle recovery by replenishing glycogen stores that are depleted during intense exercise. Glycogen is the stored form of glucose in muscles and the liver, and it is crucial for fueling exercise performance. After a workout, consuming carbohydrates helps restore glycogen and prepares the muscles for the next round of physical activity.
How Carbohydrates Aid Recovery:
- Replenishing Glycogen: Carbohydrates help restore glycogen levels, which can become depleted during exercise, especially in endurance activities like running or cycling.
- Improving Protein Synthesis: Carbohydrates promote insulin secretion, which helps drive amino acids into muscle cells and stimulates protein synthesis
- Sources of Carbohydrates: Ideal post-workout carbohydrate sources include: Whole grains (brown rice, quinoa, oatmeal), Fruits (bananas, berries, apples), Starchy vegetables (sweet potatoes, squash), Legumes (beans, lentils)
Healthy Fats: Healthy fats are essential for overall health, but they also play a role in muscle recovery. Fats help reduce inflammation and support the absorption of fat-soluble vitamins (A, D, E, and K), which are important for muscle health and recovery.
How Healthy Fats Aid Recovery:
- Reducing Inflammation: Omega-3 fatty acids, found in fatty fish (e.g., salmon) and seeds (e.g., flaxseeds, chia seeds), help reduce exercise-induced inflammation and promote muscle repair.
- Supporting Hormonal Health: Fats are essential for hormone production, including testosterone and growth hormone, both of which are important for muscle growth and recover
- Sources of Healthy Fats: Fatty fish (salmon, mackerel), Nuts and seeds, including chia seeds, walnuts, and almonds, Avocados, Olive oil, coconut oil
Vitamins and Minerals: Essential vitamins and minerals play key roles in muscle recovery by supporting various metabolic processes, such as energy production, tissue repair, and reducing oxidative stress. Some important nutrients for muscle recovery include:
- Vitamin D: Helps with calcium absorption, muscle function, and immune health.
- Magnesium: Promotes muscular relaxation and guards against spasms and cramps.
- Potassium: Crucial for proper muscle function and preventing cramps.
- Vitamin C: Important for collagen formation, which is essential for connective tissue repair.
- B vitamins: Help produce energy and lessen exhaustion.
Sources of Vitamins and Minerals:
- Vitamin D: Sunlight, fortified dairy, fatty fish
- Contains magnesium in leafy greens, whole grains, nuts, and seeds
- Potassium: Bananas, potatoes, spinach, tomato
- Vitamin C: Bell peppers, broccoli, strawberries, and citrus fruits
- B Vitamins: Whole grains, lean meats, eggs, leafy greens
Timing of nutrition for muscle recovery
The timing of your nutrition is just as important as the quality of the foods you consume. Consuming the right nutrients at strategic times can accelerate the muscle recovery process.
Pre-Workout Nutrition: Consuming a balanced meal or snack 1-2 hours before your workout provides the body with the energy it needs to perform well. This meal should contain carbohydrates for energy, moderate protein for muscle support, and a small amount of healthy fats.
Post-Workout Nutrition: Within 30-60 minutes after exercise, it’s important to consume a combination of protein and carbohydrates. This “post-workout window” is when muscles are most receptive to nutrient uptake, and consuming protein and carbs helps promote muscle repair and replenish glycogen stores.
Hydration during and after exercise: Hydrating throughout the exercise and in the period following your workout is key to supporting muscle recovery. Electrolyte-rich drinks can be beneficial after intense exercise to replace lost fluids and electrolytes.
Preventing overtraining and burnout
Overtraining, or pushing the body too hard without sufficient recovery, is one of the leading causes of muscle stiffness and injury. A well-structured training program that incorporates rest days and recovery periods is essential for preventing overtraining and ensuring that muscles can repair and rebuild effectively.
Importance of recovery days: Rest days give muscles the time they need to repair without being continuously stressed. Without proper recovery, muscles become increasingly prone to stiffness, injury, and fatigue.
Signs of overtraining: Common signs of overtraining include chronic muscle soreness, joint pain, fatigue, irritability, and sleep disturbances. If you experience these symptoms, it’s important to back off from intense exercise and allow your body to recover.
Importance of Rest in Muscle Recovery
Rest is one of the most essential components of muscle recovery and plays a pivotal role in preventing muscle stiffness, promoting overall muscle health, and enhancing athletic performance. While exercise, especially intense physical activity, is crucial for improving strength and endurance, it is during rest that the body performs the vital work of repair and regeneration. Without adequate rest, muscles become vulnerable to overuse, fatigue, and injury.
The Role of sleep in muscle recovery
Inflammatory phase: After muscle injury or microtears, inflammation occurs as the body works to clear away damaged tissue. This is a normal part of the repair process but can lead to soreness.
Repair phase: The muscle fibers begin to rebuild and repair themselves, becoming slightly stronger and more resilient.
Growth phase: After adequate rest, the repaired muscle fibers grow larger and stronger, improving overall strength and performance.
Sleep is an often overlooked but crucial factor in the muscle recovery process. While exercise is necessary for stimulating muscle growth and enhancing performance, it is during sleep that the body carries out vital repair and regeneration processes. Without adequate sleep, the muscles cannot recover properly, leading to increased muscle stiffness, soreness, fatigue, and a higher risk of injury. the impact of sleep deprivation on muscle health, and strategies to improve sleep quality for optimal recovery.
Protein Synthesis: During sleep, the body increases protein synthesis, which is the process of building new proteins from amino acids. This is essential for repairing muscle fibers that have been broken down during exercise. Growth hormone, which is released in greater quantities during deep sleep, plays a significant role in stimulating protein synthesis and muscle repair.
Muscle Repair and Regeneration: When muscles undergo stress during exercise, small tears, or microtears, occur in muscle fibers. Sleep accelerates the repair of these fibers, helping them heal and grow back stronger. Without sleep, this repair process is delayed or incomplete, leading to muscle stiffness, soreness, and compromised performance.
Hormone Regulation: Sleep plays a key role in regulating the levels of various hormones that influence muscle recovery. For example:
- Growth Hormone (GH): Growth hormone levels peak during deep sleep. This hormone plays a critical role in muscle tissue repair, fat metabolism, and overall recovery. GH helps promote muscle growth by stimulating the regeneration of damaged tissues and the synthesis of proteins.
- Testosterone: Testosterone, a hormone essential for muscle growth and recovery, is also released during sleep. Lack of sleep can lower testosterone levels, hindering the muscle recovery process and potentially leading to muscle atrophy over time.
- Cortisol: Cortisol is a stress hormone that, if elevated for prolonged periods (such as during sleep deprivation), can impair muscle recovery. High cortisol levels can lead to muscle breakdown and inflammation, making proper sleep essential to managing cortisol levels.
- Energy Restoration: Sleep allows for the restoration of glycogen stores in muscles. Glycogen is the body’s primary energy source during exercise, and sleep helps replenish these energy reserves. Without adequate sleep, the muscles may remain in a depleted state, which can cause muscle fatigue and increase the risk of injury during subsequent workouts.
The stages of sleep and their impact on muscle recovery
Sleep is divided into different stages, each of which serves a unique purpose. Two key stages of sleep play a direct role in muscle recovery:
Deep Sleep (Slow-Wave Sleep): Deep sleep, also known as slow-wave sleep (SWS), is the most important stage for muscle recovery. During this stage, the body undergoes the most intensive repair and regeneration. Growth hormone is released in high amounts during deep sleep, which helps stimulate muscle repair, reduce inflammation, and promote tissue regeneration. This stage is also where the body focuses on restoring energy stores in the muscles.
Rapid Eye Movement (REM) Sleep: While REM sleep is typically associated with brain function and mental recovery, it still plays an indirect role in muscle recovery. REM sleep helps with emotional regulation, memory consolidation, and cognitive functions, which are crucial for overall well-being. Mental recovery and reduced stress levels can positively affect physical recovery as well.
Sleep deprivation’s effects on muscular recovery
Chronic sleep deprivation or poor sleep quality can significantly impair muscle recovery and lead to various negative outcomes for both physical and mental health. Some of the consequences of inadequate sleep on muscle recovery include:
Impaired Muscle Repair: Without enough sleep, the body does not have the necessary time to repair and rebuild muscle tissue. Microtears in muscle fibers remain unrepaired, leading to prolonged soreness, stiffness, and a slower recovery process. Incomplete muscle recovery can also lead to muscle weakness and a higher risk of injury.
Decreased Protein Synthesis: Sleep deprivation lowers the rate of protein synthesis, meaning the muscles cannot rebuild effectively after exercise. This can hinder muscle growth, slow down recovery time, and ultimately affect overall performance.
Increased Cortisol Production: sleep deprivation leads to an increase in cortisol levels, a hormone that promotes muscle breakdown. Elevated cortisol levels not only interfere with muscle recovery but also impede fat loss and increase the likelihood of gaining weight around the midsection. High cortisol levels also interfere with sleep quality, creating a cycle of stress and poor recovery.
Reduced Strength and Performance: Insufficient sleep negatively impacts both strength and endurance. Lack of sleep leads to fatigue, which reduces the body’s ability to perform optimally during physical activity. Muscle strength, endurance, reaction times, and focus are all compromised, reducing athletic performance and increasing the chance of injury.
Increased Risk of Injury: Sleep-deprived muscles are more prone to injury because they are not fully recovered and are still in a state of repair. Sleep deprivation also affects coordination, motor skills, and balance, all of which contribute to the risk of strains, sprains, and other injuries .
Tips for improving sleep quality for muscle recovery
To maximize the benefits of sleep for muscle recovery, it is important to adopt healthy sleep habits. Here are some strategies to improve sleep quality and enhance muscle recovery:
- Create a Consistent Sleep Schedule: Try to go to bed and wake up at the same time every day, even on weekends. This helps regulate the body’s internal clock and improves the quality of sleep.
- Avoid Stimulants: Limit the intake of caffeine, nicotine, and other stimulants, especially in the afternoon or evening, as they can interfere with sleep quality.
- Establish a Calm Nighttime Routine: Before going to bed, do something soothing, like reading, meditation, or a warm bath. These exercises assist in letting your body know when it’s time to relax.
- Be Your Sleeping Space Relaxed: be sure that your bedroom is dark, quiet, and cool. To produce the ideal sleeping environment, think about utilizing earplugs, blackout curtains, or a white noise machine.
- Avoid Heavy Meals Before Bed: Eating large or heavy meals right before sleep can disrupt digestion and make it harder to fall asleep. If you’re hungry, opt for a small, light snack.
- Limit Screen Time: The blue light emitted by smartphones, tablets, and computers can interfere with the production of melatonin, a hormone that helps regulate sleep. Give yourself at least an hour before bed to avoid utilizing screens.
Stress management techniques to prevent muscle stiffness
Chronic stress is one of the primary contributors to muscle tension, discomfort, and stiffness. When the body is under stress, it triggers a “fight or flight” response, causing muscles to tighten, particularly in areas such as the neck, shoulders, and back. This continuous muscle contraction can result in stiffness and pain. Learning effective stress management techniques can help relax the body, reduce muscle tightness, and improve overall well-being. Here are several stress management techniques that can significantly reduce muscle stiffness and promote relaxation.
Mindfulness and Meditation
Mindfulness and meditation are powerful tools for reducing stress and relieving muscle tension. Both practices help you become aware of the present moment, reducing mental chatter and allowing your body to relax.
How they help with muscle stiffness:
Reduces Cortisol Levels: Mindfulness and meditation have been shown to reduce the production of cortisol, the hormone associated with stress. Lower cortisol levels can help decrease muscle tension and stiffness.
Increases Relaxation: Meditation activates the parasympathetic nervous system, the body’s relaxation response, which counteracts the stress-induced “fight or flight” response. This results in reduced muscle tension and improved circulation.
Techniques to practice:
Breathe mindfully by paying attention to your breath and taking deep breaths through your nose and mouth. This simple exercise can help bring awareness to your body and promote relaxation.
Guided Meditation: Use guided meditation apps or videos to lead you through relaxation exercises. These often focus on body scans, where you mentally relax and release tension in different areas of your body.
Body Scan Meditation: Starting from your toes and working your way up to your head, mentally check in with each part of your body, focusing on any areas of tension and consciously relaxing them.
Deep Breathing Exercises
One of the easiest and most efficient methods of stress management is deep breathing. It helps activate the parasympathetic nervous system, which is responsible for promoting a state of calm and relaxation.
How it Helps with muscle stiffness:
Increases Oxygen Supply: Deep breathing increases the amount of oxygen entering the body, which can help relax tight muscles and reduce stiffness.
Reduces Muscle Tension: Breathing deeply signals the body to relax, which helps release the muscle contractions that often occur during stress.
Calms the Nervous System: Deep breathing slows the heart rate and reduces blood pressure, promoting a feeling of calmness and easing muscle tension.
Techniques to practice:
Diaphragmatic Breathing: Locate a cozy sitting or lying position. One hand should be placed on your chest, and the other on your abdomen. Take a deep breath through your nose, making sure your abdomen rises, not your chest. Exhale slowly through your mouth. Repeat for several minutes.
4-7-8 Breathing: Inhale through your nose for 4 counts, hold your breath for 7 counts, and exhale slowly through your mouth for 8 counts. This technique helps calm the mind and body, relieving stress and muscle tension.
Progressive Muscle Relaxation (PMR)
The approach known as Progressive Muscle Relaxation (PMR) entails tensing and then relaxing various bodily muscle groups. By systematically relaxing your muscles, you can reduce overall tension and improve your awareness of where you hold stress.
How It Helps with Muscle Stiffness:
Reduces Muscle Tension: PMR allows you to release physical tension by intentionally tightening and relaxing muscles, which helps relieve stiffness.
Increases Body Awareness: It helps you become more aware of where you carry tension, allowing you to consciously release it before it builds into more severe stiffness.
How to Practice PMR:
Find a Quiet Space: Sit or lie in a comfortable position in a quiet space where you won’t be disturbed.
Start with Your Feet: Tense the muscles in your feet for 5-10 seconds, then release and relax them completely for 20-30 seconds.
Work Your Way Up: Move through different muscle groups, including your calves, thighs, abdomen, chest, hands, arms, shoulders, neck, and face. For each muscle group, tense for a few seconds, then release.
Focus on Relaxation: As you release tension, focus on the sensation of relaxation and allow your body to soften.
Yoga and Tai Chi
Yoga and Tai Chi are both mind-body practices that involve gentle movements, controlled breathing, and meditation. These practices are highly effective in reducing stress and muscle stiffness, promoting relaxation, and improving flexibility.
How they help with muscle stiffness:
Improves Flexibility: Both yoga and Tai Chi emphasize movement and stretching, which helps release tight muscles and improves joint flexibility.
Promotes Mind-Body Connection: These practices encourage mindfulness, teaching you to focus on your breath and body, reducing mental and physical stress.
Balances the Nervous System: The slow, deliberate movements help calm the nervous system, reducing muscle tension and stress.
Yoga Poses to Relieve Stress and Muscle Stiffness:
Child’s Pose (Balasana): Kneel on the floor, lower your torso to the ground, and extend your arms in front of you. This pose encourages relaxation by gradually stretching the hips and back.
Cat-Cow Pose (Marjaryasana-Bitilasana): On all fours, alternate between arching your back (cow pose) and rounding your spine (cat pose). This movement helps relieve tension in the spine, neck, and shoulders.
Downward Dog (Adho Mukha Svanasana): This pose stretches the hamstrings, calves, and spine, helping to alleviate stiffness and improve flexibility.
Tai Chi Movements to Relieve Stress:
Wave Hands Like Clouds: This slow, flowing movement helps release tension in the upper body, especially in the shoulders and neck.
Tai Chi Breathing: Deep breathing combined with slow, deliberate movements helps relax the mind and body, reducing overall muscle stiffness.
Visualization and Guided Imagery
Visualization involves mentally imagining a peaceful and relaxing scene or situation. This technique can help reduce stress by shifting focus away from stressful thoughts and encouraging a relaxed state of mind.
How It Helps with Muscle Stiffness:
Reduces Stress: By focusing on calming images, you activate the relaxation response, which helps reduce muscle tension.
Improves Mental Focus: Visualization helps break the cycle of stress and worry, which can contribute to muscle stiffness and pain
How to Practice Visualization:
- Choose a Comfortable Position: Take a seat or lie down in a peaceful, cozy area.
- Close Your Eyes and Breathe: Focus on your breath and slow your breathing to calm the nervous system.
- Create a Peaceful Mental Image: Imagine a relaxing scene, such as a calm beach, a peaceful forest, or a beautiful meadow. Visualize yourself experiencing the sights, sounds, and sensations of this peaceful environment.
- Focus on Muscle Relaxation: While immersed in the scene, imagine your muscles softening and relaxing, releasing all tension. Allow your body to feel light and free of stiffness.
Cognitive Behavioral Approaches:
Cognitive-behavioral therapy (CBT): CBT can help individuals identify and address the underlying thoughts and patterns that contribute to anxiety and stress. By reducing the psychological triggers of muscle tension, individuals can experience relief from physical symptoms.
Innovative Therapies
New and emerging therapies for muscle stiffness are also being investigated:
- Botulinum Toxin (Botox): Botox has been used to treat spasticity in conditions like cerebral palsy and multiple sclerosis. Ongoing studies are exploring new, more effective uses for Botox in treating muscle stiffness in various conditions.
- Gene Therapy: Researchers are exploring the potential of gene therapies to treat muscle stiffness caused by genetic disorders like muscular dystrophy. By targeting the underlying genetic causes of muscle stiffness, these therapies could provide long-term solutions.
- Wearable Technology: Wearables that monitor muscle stiffness and provide real-time feedback are becoming an area of interest. These devices can track muscle tension and suggest interventions to reduce stiffness, potentially improving both athletic performance and quality of life for individuals with chronic conditions.
How much sleep is required to restore muscles?
The optimal amount of sleep required for muscle recovery varies based on several factors, including individual needs, age, and the intensity of physical activity. Nonetheless, the standard advice for the majority of individuals is
7-9 hours of sleep per night for adults, including athletes, to ensure proper muscle recovery and overall health.
Athletes and highly active individuals may need more sleep, potentially up to 10 hours per night, especially during periods of intense training or competition.
It’s important to remember that the quality of sleep is just as important as the quantity. Disruptions in sleep cycles, such as waking up frequently or having trouble falling asleep, can compromise muscle recovery. Prioritizing both the duration and quality of sleep is essential for optimal recovery.
FAQS
How long does muscle stiffness last?
Muscle stiffness typically lasts for a few hours to a couple of days, depending on the severity and cause. If it persists longer, it may indicate an underlying condition that requires medical attention.
Is muscle stiffness normal after exercise?
Yes, muscle stiffness after exercise is common, especially if you’ve engaged in intense physical activity or tried new exercises. This is known as Delayed Onset Muscle Soreness (DOMS) and usually peaks 24-48 hours after activity.
Can dehydration cause muscle stiffness?
Yes, dehydration can contribute to muscle stiffness because muscles need proper hydration to function efficiently. Dehydration can lead to cramps, spasms, and tightness in muscles
When should you see a doctor for muscle stiffness
if muscle stiffness is severe, persistent, or accompanied by swelling, redness, weakness, or other unusual symptoms, it’s a good idea to see a doctor. It may indicate an underlying medical condition such as a muscle injury or nerve problem.
Can stress lead to muscle stiffness?
Yes, stress can cause muscle tension, often resulting in stiffness,
particularly in the neck, shoulders, and back. Practicing relaxation
techniques, such as deep breathing or yoga, can help reduce
stress-induced muscle stiffness.
Does age affect muscle stiffness?
Yes, as people age, their muscles may become stiffer and less flexible due to changes in muscle mass, collagen production, and joint mobility. Regular exercise, stretching, and maintaining a healthy lifestyle can help reduce the impact of aging on muscle stiffness.
Can a deficiency of hydration and nutrition cause muscle stiffness?
Yes, a deficiency in hydration and proper nutrition can contribute to muscle stiffness. Dehydration depletes the body’s fluids needed for muscle function, and inadequate nutrient intake can lead to deficiencies in minerals like magnesium and calcium, which are crucial for muscle contraction and relaxation
Does poor posture lead to muscle stiffness?
Yes, poor posture can directly lead to muscle stiffness, as it causes certain muscles to become overactive and strained, leading to tightness and tension, particularly in the neck, shoulders, and upper back, when maintained for extended periods. this can result in discomfort and pain due to muscle imbalances created by improper alignment.
Is ergonomic advice mandatory after recovery from muscle stiffness?
Yes, ergonomic advice is highly beneficial after recovering from muscle stiffness to help prevent future occurrences and promote long-term muscle health.
What is the advantage of using trigger point therapy in muscle stiffness?
The primary advantage of using trigger point therapy for muscle stiffness is its ability to directly target and release tight muscle fibers within specific areas called “trigger points,” which are often the source of pain and discomfort, leading to a significant reduction in muscle tension and improved flexibility and range of motion.
Is it safe to use cupping therapy for muscle stiffness?
By reducing muscle stiffness at the right cupping intensities, cupping therapy can help athletes perform better and experience less discomfort and tiredness.
References
- Professional, C. C. M. (2025, February 7). Muscle stiffness. Cleveland Clinic. https://my.clevelandclinic.org/health/symptoms/25147-muscle-stiffness
- Seymour, T. (2023, October 24). What causes muscle soreness and stiffness? https://www.medicalnewstoday.com/articles/320545
- PhysioTattva. (n.d.). Relieve muscle stiffness: Symptoms, causes, and solutions. https://www.physiotattva.com/symptoms/muscle-stiffness
- Clinic, O. (2024, April 5). Muscle stiffness. The Orthopedic Clinic. https://orthotoc.com/muscle-stiffness/
- Cht, A. B. P. D. (2024, October 18). Why are my muscles stiff? Verywell Health. https://www.verywellhealth.com/muscle-stiffness-symptoms-causes-and-treatment-5525837
- CARE Hospitals. (n.d.). CARE hospitals. https://www.carehospitals.com/symptoms/muscle-stiffness
- Muscle stiffness – Symptoms, causes, diagnosis & treatment. (n.d.). https://www.medicoverhospitals.in/symptoms/muscle-stiffness
- Seidenburg, M. (2025, January 31). Causes of muscle stiffness & treatments. BenchMark Physical Therapy. https://www.benchmarkpt.com/blog/causes-of-muscle-stiffness-treatments/
- Narayana Health. (n.d.). Narayana Health. https://www.narayanahealth.org/blog/muscle-stiffness-causes-and-treatment
- What deficiency causes muscle stiffness? (n.d.). https://www.avogel.co.uk/health/muscles-joints/stiffness/what-deficiency-causes-muscle-stiffness
- Wong, A. (2022, February 8). Why do my muscles feel stiff? | Myphysio Health Clinics. Myphysio Health Clinics. https://my-physio.com.au/why-do-my-muscles-feel-stiff/


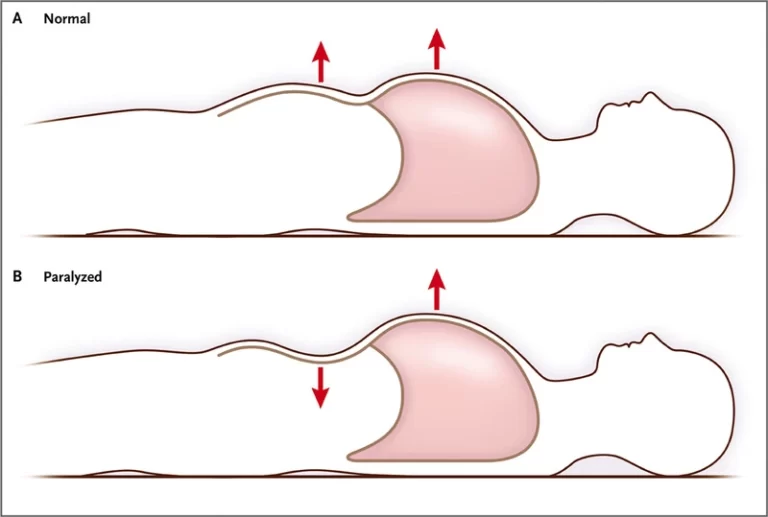
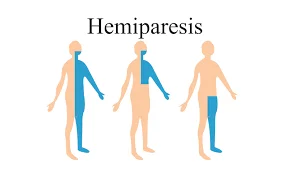

7 Comments