Lumbar Degenerative Disc Disease
Table of Contents
What is a Lumbar Degenerative Disc Disease?
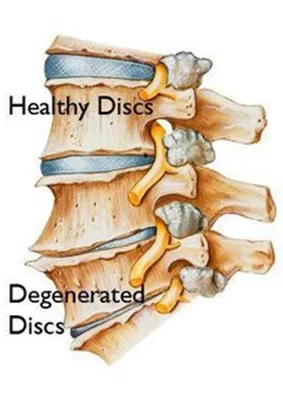
Lumbar degenerative disc disease is a chronic condition that affects the spine. It is most commonly found in older individuals and is characterized by changes in the intervertebral discs, which are the shock absorbers of the spine. The discs become less elastic with age, and are subject to wear and tear due to factors such as poor posture, obesity, and repetitive stress. Over time, this degeneration can lead to pain in both the back and legs and loss of strength and flexibility.
Degenerative disc disease is not really a disease but a term used to describe the normal changes in your spinal discs as you age.
Spinal discs are soft, compressible discs that separate the interlocking bones (vertebrae) that make up the spine. The discs act as shock absorbers for the spine, allowing it to flex, bend, and twist. Degenerative disc disease can take place throughout the spine, but it most often occurs in the discs in the lower back (lumbar region) and the neck (cervical region).
ANATOMY OF DISC
The Intervertebral Disc (IVD) consists of three distinct components
- A central nucleus pulposus
- A peripheral annulus fibrosus
- Two vertebral endplates
Nucleus Pulposus: a gel-like mass composed of water and proteoglycans held by randomly arranged fibres of collagen.
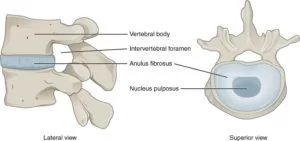
it’s water-attracting properties, any attempt to deform the nucleus causes the applied pressure to be dispersed into various directions, similar to a person on a waterbed.
Annulus Fibrosus: consists of “lamellae” or concentric layers of collagen fibers. The fibre orientation of each layer of lamellae alternate and therefore allow effective resistance of multidirectional movements.
Vertebral endplate: a plate of cartilage that acts as a barrier between the disc and the vertebral body. They cover the superior and inferior aspects of the annulus fibrosus and the nucleus pulposus.
Symptoms:
- Low Back Pain that ranges from nagging to severe and disabling
- Numbness and tingling in the extremities
- Pain that affects the low back, buttocks, and thighs
- Weakness in the leg muscles or foot drop may be a sign that there is damage to the nerve root
- Pain in the neck that may radiate to the arms and hands
- Pain is worse when sitting
- Pain gets worse when bending, lifting, or twisting
- Periods of severe pain that come and go, lasting from a few days to a few months
- Pain lessens when walking and moving
- Pain that lessens with changing positions often or lying down
Causes of Lumbar Degenerative Disc Disease
The drying out of the disc. When we are born, the disc is about 80 percent water. As we age, the disc dries out and doesn’t absorb shocks as well.
Daily activities and sports, which cause tears in the outer core of the disc. By age 60, most people have some degree of disc degeneration. Not everyone at that age has back pain, however.
Injuries, can cause swelling, soreness and instability. This can result in low back pain.
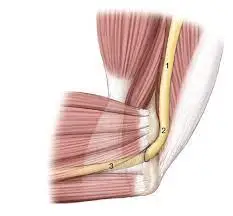
Inflammation, as the proteins in the disc space, irritate the surrounding nerves—both the small nerve within the disc space and potentially the larger nerves that go to the legs (the sciatic nerve).
Abnormal micro-motion instability, when the outer rings of the disc, called the annulus fibrosis, are worn down and cannot absorb stress on the spine effectively, resulting in movement along the vertebral segment.
Treatment of Lumbar Degenerative Disc Disease
Pain relieving medications. Pain medications such as NSAIDs, ibuprofen (Advil), or naproxen (Aleve) can relieve inflammation that contributes to discomfort, stiffness, and nerve root irritation. Acetaminophen (Tylenol) is a pain reliever that interferes with pain signals sent to the brain.
Epidural steroid injections (ESIs). A steroid injection administered in the space surrounding the spine can reduce pain signals as well as inflammation. A steroid injection may be used in combination with a physical therapy program to provide pain relief during exercise and rehabilitation. When effective, an epidural steroid injection may alleviate pain for a couple weeks up to one year.
SURGERY
SPINAL FUSION
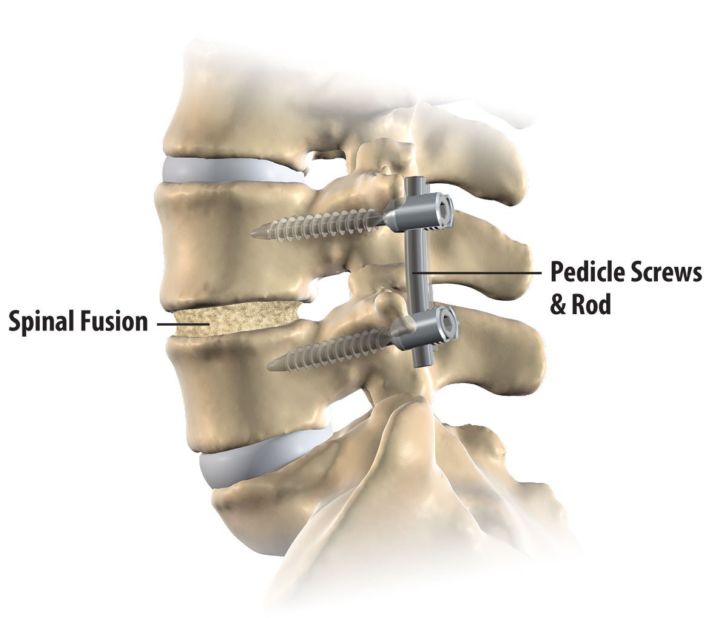
A lumbar spine fusion is a type of back surgery designed to treat low back pain from degenerative disc disease. It is called a “spine fusion” because the surgery involves placing small morsels of bone either in the front of the spine (in the disc space) and/or along the back of the spine (in the posterolateral gutter) so that the bone grows together and fuses that section of the spine.
The fusion is designed to eliminate motion in that fused segment of the spine, thereby decreasing or eliminating the back pain created by the motion. The spine is not actually fused at the time of the surgery. Instead, the surgery creates the conditions for the spine to be able to fuse and the fusion is a process that will set up over a 3 to 6-month (and up to 18 months) period of time following the spinal fusion surgery
Lumbar artificial disc replacement:
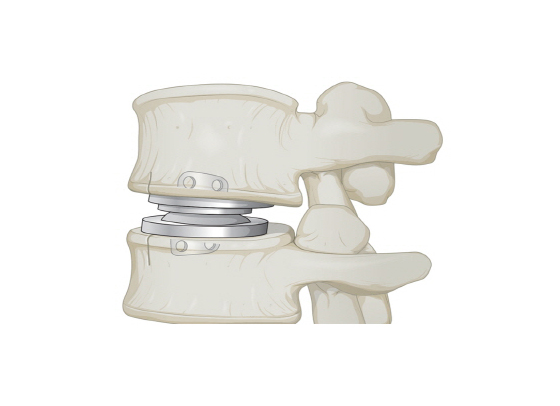
In this procedure, the symptomatic lumbar disc is removed and then replaced with an artificial disc designed to maintain the natural movement in the spine. A lumbar artificial disc replacement seeks to minimize pain by reducing instability and muscle tension caused by painful micro-motions at the degenerated disc level.
Physical Therapy Treatment:
To treat lumbar degenerative disc disease, it is important to find the source of the pain. The pain can be due to a bulging, herniated, or degenerated disc. Treatment of lumbar degenerative disc disease depends on the source of pain and treatment of the other conditions that can cause the pain. Treatment for lumbar degenerative disc disease can include physical therapy and other treatment options.
Heat and ice.: Applying heat to the low back improves circulation, which reduces muscle spasms and tension and improves mobility. Ice packs can reduce inflammation and numb mild pain. It can be helpful to apply heat before physical activities to relax the muscles, and to apply ice after activity to minimize inflammation.
Lumbar traction: By stretching the back, spinal traction works to alleviate pain caused by muscle tightness or compressed nerves. The therapist can do that manually (by using his or her own body) or mechanically (with special machines). Especially if your nerve is being pinched by the foramen—the area where the nerve exits the spinal canal—your therapist may try traction. It’s thought to widen the foramen by stretching the spine to readjust the vertebrae.
Interferential Therapy (IFT): A low frequency electrical current is used to stimulate your muscles to reduce inflammation.
Ultrasound Therapy: Ultrasound may help reduce muscle spasms, stiffness, and pain by sending sound waves deep into your muscle tissues. This creates a gentle heat that enhances circulation.
EXERCISE
Hamstring Stretch

lying flat on your back with both legs flat on the floor.
Next, bring your right knee towards your body and support your right thigh with your hands—or wrap a towel around your thigh and firmly hold each end of the towel.
Raise your right foot towards the ceiling with the goal of placing your right leg in a perpendicular position. You can gently pull on the towel to bring your leg closer to your body.
Hold this position for 30 seconds, and then repeat on your opposite leg.
Pelvic Tilt exercise :
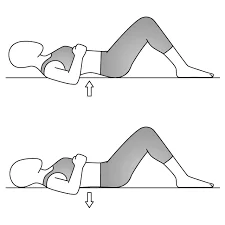
Lie on your back with your feet flat on the floor.
As you exhale, squeeze your abdominal muscles, push your belly button toward the floor, and flatten your low back.
Hold for 5 seconds. Relax.
Repeat 10 times, holding for 5 seconds each time.
Knee to Chest exercise
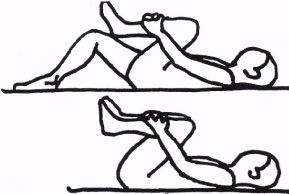
Lie on your back with feet flat on the floor.
Bring your right knee toward your chest, using your hands to hold your leg in the stretched position. Hold for 10 seconds.
Lower your right leg and repeat the exercise with the left knee. Hold for 10 seconds.
Repeat with each leg 3 to 5 times.
After stretching each leg individually, perform the exercise by holding both knees in the stretched position. Hold for 10 seconds and repeat 3 to 5 times.

Lower Trunk Rotation
Lie on your back in the hook-lying position (knees bent and feet flat on the floor).
Rotate your knees to 1 side, holding them for 3 to 5 seconds.
While contracting your abdominal muscles, slowly rotate your knees to the other side and hold for 3 to 5 seconds.
Repeat up to 10 times on both sides.
DO’S and DON’TS:
- Position your computer properly. You should be seated at eye level to your screen, so that you don’t have to look too far down or too far up to do your work.
- Getting the right mattress. No matter how comfortable a squishy-soft feather bed may seem at first, a firmer mattress is usually the best for your back, Polivka says. “The types of beds where partners can choose a different level of support can be good, because differences in body structure and size can make what’s comfortable for one person different from another.”
- Don’t push yourself too hard. Respect your body and its limits. Avoid re-injuring yourself by listening to what your body is telling you during exercise. Sitting tends to be especially bothersome for many people with disc-related back pain.




One Comment