BIOFEEDBACK USE IN PHYSIOTHERAPY
DEFINATION
Biofeedback is a technique you can use to learn to control some of your body’s functions, such as your heart rate. During biofeedback, you’re connected to electrical sensors that help you receive information about your body. This feedback helps you make subtle changes in your body, such as relaxing certain muscles, to achieve the results you want, such as reducing pain. In essence, biofeedback gives you the ability to practice new ways to control your body, often to improve a health condition or physical performance.
Table of Contents
Types of biofeedback
Your therapist might use a variety of biofeedback methods depending on your health problems and goals. Biofeedback
types include
- Brain waves.
This type uses scalp sensors to monitor your brain waves using an electroencephalograph (EEG).
2. Breathing.
During respiratory biofeedback, bands are placed around your abdomen and chest to monitor your breathing patterns and respiration rate.

3. Heart rate.
This type uses finger or earlobe sensors with a device used to detect blood volume changes (photoplethysmograph). Or sensors placed on your chest, lower torso or wrists use an electrocardiograph (ECG) to measure your heart rate and how your heart rate varies.

4. Muscle contraction.
This type involves placing sensors over your skeletal muscles with an electromyograph (EMG) to monitor the electrical activity that causes muscle contraction.

5. Sweat gland activity.
Sensors attached around your fingers or on your palm or wrist with an electrodermograph (EDG) measure the activity of your sweat glands and the amount of perspiration on your skin, alerting you to anxiety.
6. Temperature.
Sensors attached to your fingers or feet measure blood flow to your skin. Because your temperature often drops when you’re under stress, a low reading can prompt you to begin relaxation techniques.
Biofeedback devices
You can receive biofeedback training in physical therapy clinics, medical centers, and hospitals. A growing number of biofeedback devices and programs also are being marketed for home use, including:
1) Interactive computer programs or mobile devices.
Some types of biofeedback devices measure physiological changes in
your body, such as your heart rate activity and skin changes, by using one or more sensors attached to your fingers or your ear. The sensors plug into your computer.
Using computer graphics and prompts, the devices then help you master stress by helping you to pace your breathing, relax your muscles, and think positive self-statements about your ability to cope. Studies show that these types of devices might be effective in improving responses during stress and inducing feelings of calm and well-being.
Another type of biofeedback therapy involves wearing a headband that monitors your brain activity while you meditate. It uses sounds to let you know when your mind is calm and when it’s active to help you learn to control your stress response. The information from each session can be stored on your computer or mobile device so that you can track your progress over time.
2) Wearable devices.
One type involves wearing a sensor on your waist that monitors your breathing and tracks your breathing patterns using a downloadable app. The app can alert you if you’re having prolonged tension, and it offers guided breathing activities to help restore your calm.
The Food and Drug Administration (FDA) has approved a biofeedback device, Resperate, for reducing stress and lowering blood pressure. Resperate is a portable electronic device that promotes slow, deep breathing.
However, the FDA doesn’t regulate many biofeedback devices marketed for home use. Before trying biofeedback therapy at home, discuss the types of devices with your care team to find the best fit.
Be aware that some products might be falsely marketed as biofeedback devices, and that not all biofeedback practitioners are legitimate.
3) Neuromuscular biofeedback
The neuromuscular system is the nervous and musculoskeletal system working together to produce movement. Any measure of these systems can be used to provide neuromuscular biofeedback. Neuromuscular biofeedback methods used in physical rehabilitation include EMG biofeedback and real time ultrasound imaging (RTUS) biofeedback.
4) Electromyography (EMG) biofeedback
EMG biofeedback is a method of retraining muscle by creating new feedback systems as a result of the conversion of myoelectrical signals in the muscle into visual and auditory signals. EMG uses surface electrodes to detect a change in skeletal muscle activity, which is then fed back to the user usually by a visual or auditory signal. EMG biofeedback can be used to either increase activity in weak or paretic muscle or it can be used to facilitate a reduction in tone is a spastic one. EMG biofeedback has been shown to be useful in both musculoskeletal and neurological rehabilitation.
Draper and Ballard suggested that EMG biofeedback is more effective in facilitating the recovery of quadriceps femoris muscle peak torque than electrical stimulation treatment in participants post anterior cruciate ligament reconstruction. Early reports highlighted EMG biofeedback as an efficacious therapeutic modality following menisectomy. A recent randomized,single blind, clinical study suggested that the addition of EMG biofeedback to a conventional exercise programme resulted in a significantly shorter time in using a walking aid compared to conventional exercise training alone following arthroscopic partial meniscectomy. In addition, the EMG biofeedback group demonstrated significantly better quadriceps femoris muscle strength and Lysholm Knee Scoring Scale scores than the home exercise and electrical stimulation groups. Similar results were found by Kirnap et al. , who also compared the effects of home exercise and EMG biofeedback after arthroscopic meniscectomy and found a significant increase in Lysholm Knee Scoring Scale score, knee flexion angle, quadriceps femoris muscle activity and power in the group which received EMG biofeedback. However a recent study which compared a strengthening exercise program with EMG biofeedback to the same exercise program with no biofeedback demonstrated no significant additive effect of EMG biofeedback in participants with knee osteoarthritis. While the use of
EMG biofeedback in these populations appears promising, further work is required as the studies discussed were small scale studies.
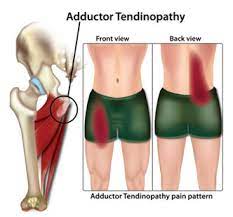
EMG biofeedback has been advocated by McConnell as a training procedure that could be used during quadriceps exercises to equalize vastus medialis and vastus lateralis muscle activity. However the value of EMG biofeedback in the treatment of patellofemoral pain syndrome is questionable. Early reports suggested that EMG biofeedback coupled with an exercise programme was an effective treatment in patients with patellofemoral pain syndrome, however Dursun and colleagues found that EMG biofeedback did not produce further clinical improvement when compared with a
conventional exercise program. Yip and Ng also demonstrated that the addition of EMG biofeedback on vastus medialis obliquus activity had no measurable effect after treatment. More recently however, NG and colleagues found that EMG biofeedback was an effective adjunct to therapeutic exercise for patients with patellofemoral pain syndrome.
Further work examining the application of EMG biofeedback in the treatment of patellofemoral pain is warranted to investigate these conflicting reports.
The results of three randomised controlled trials (RCTs) suggest that EMG biofeedback may be useful in conditions of muscular tension to facilitate a reduction in neck muscle activation and therefore decrease pain. Dellve and colleagues in their RCT of female workers on long-term sick leave with chronic neck pain found that an EMG biofeedback intervention was associated with increased vitality and increased performance in functional testing. More recently, Ma et al. compared EMG biofeedback, active exercise, passive treatment and a no treatment control in the treatment of work-related neck and shoulder pain. The results of this study suggest that EMG biofeedback produced a generalized relaxation effect in the neck
and shoulder muscles, which was not found in the other intervention groups. Voerman and colleagues compared ambulant
EMG biofeedback and ergonomic counselling to ergonomic counselling alone on work-related neck and shoulder pain and
disability and found that while both groups showed significant reductions in self reported pain intensity and disability there
was however no difference between the groups. These positive findings advocate the use of EMG biofeedback to facilitate a reduction in muscular tension and therefore decrease pain.
The efficacy of EMG biofeedback as a treatment for individuals with chronic whiplash-associated disorders is however vague.Voerman et al. in a small clinical study, observed that four weeks of ambulant EMG biofeedback training for the upper trapezius muscles may be beneficial in reducing pain and disability levels and normalizing muscle activation patterns in chronic whiplash-associated disorder participants. The results of the study conducted by Ehrenborg and Archenholtz however did not support the use of EMG biofeedback of the upper trapezius muscle as an adjunct to an interdisciplinary rehabilitation programme for people with chronic whiplash-associated disorders.
Extensive research has been conducted examining the efficacy of EMG biofeedback in the rehabilitation of patients with hemiplegia following cardiovascular accident (CVA) . Armagan and colleagues demonstrated the potential benefits of EMG biofeedback in conjunction with exercise in maximising hand function in hemiplegic patients. The results of a study performed by Aiello and colleagues suggested that treadmill gait retraining augmented with EMG biofeedback facilitates improvements in gait function in post CVA participants. Inglis et al. showed that compared to conventional
therapy, EMG biofeedback resulted in greater improvements in functional properties such as muscle force, active range of movement and motor recovery in hemiplegic patients. However a systematic review concluded that EMG biofeedback has no effect in improving joint range of motion, functional ability, or stride length or gait speed following CVA, however
there is some evidence of improvements in gait quality assessments, range of motion at the shoulder and restoration of motor power. Further work has been conducted in this field since the publication of this review, therefore further systematic reviewing of this topic is warranted.
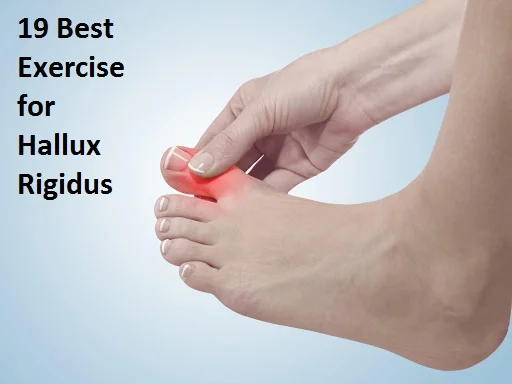
Several researchers have investigated the application of EMG biofeedback to modify gait in children with cerebral palsy (CP). Early reports suggest that EMG biofeedback of triceps surae muscle activity during gait may be efficacious in improving gait symmetry in children with CP. A preliminary study showed that two children diagnosed with CP who used EMG biofeedback demonstrated improved toe clearance during the swing phase of gait and a newly learned ability to recruit and relax the anterior tibialis. Dursun and colleagues also evaluated the effectiveness of biofeedback
treatment on gait function in children with CP. This larger study included thirty-six children with cerebral palsy who were randomly assigned to receive either EMG biofeedback and exercise or exercise only. The results of this study showed that children who received biofeedback showed significant improvements in muscle tone and ankle range of movement,
compared to children who received the exercise programme only. Gait showed statistically significant progress in both groups, but the biofeedback group was superior to the exercise only group. A recent study by Bloom and colleagues examined whether the prolonged use of EMG biofeedback could improve upper extremity function in children with CP. This small investigation demonstrated promising results, suggesting that further testing of prolonged EMG biofeedback in this population is warranted.
EMG biofeedback is the most widely used and widely reported method of biofeedback. However, the limited number of large RCTs and systematic reviews means further work is required. Nevertheless the existing evidence for the use of EMG biofeedback in musculoskeletal and neurological rehabilitation appears promising.
Indication
There are many indications for biofeedback. Stress urinary incontinence is an indication for biofeedback. We found in the literature that the addition of biofeedback to the training of the pelvic floor muscles for the treatment of stress urinary incontinence improved pelvic floor muscles function, reduced urinary symptoms, and improved of the quality of life.
Pelvic floor muscle exercises and biofeedback are also an effective treatment for men with erectile dysfunction.
If we search evidence for biofeedback as the treatment for headaches we found that biofeedback-related approaches to headache therapy fall into two broad categories: general biofeedback techniques (often augmented by relaxation-based strategies) and methods linked more directly to the pathophysiology underlying headache.
Further we found that EMG therapy is useful in enhancing knee extension after an ACL reconstruction but only in the early phase of the rehabilitation after the reconstruction.
The use of general biofeedback-assisted relaxation techniques for headache has been evaluated extensively. We can conclude that:
Various forms of biofeedback are effective for migraine and tension-type headache;
Outcomes with biofeedback rival outcomes with medication therapy; Combining biofeedback with medication can enhance outcomes;
Despite efficacy in many patients, biofeedback fails to bring significant relief to a sizeable number of headache patients.
Biofeedback methods that more directly target headache pathophysiology have focused chiefly on migraine and tension-type headache. These headache-specific approaches include blood volume pulse biofeedback, which has considerable supportive evidence, and electroencephalographic feedback.For tension-type headache we found that biofeedback was
more effective than headache monitoring, placebo, and relaxation therapies. The strongest improvements were found for frequency of headache episodes. Further significant effects were observed for muscle tension. Biofeedback is also used for patients with migraine. This treatment is found effective to reduce the number of headaches per week but there
were no change in intensity, disability and length of headache.
Biofeedback, sometimes called biofeedback training, is used to help manage many physical and mental health issues,
including:
Biofeedback appeals to people for a variety of reasons:
Anxiety or stress
Asthma
Attention-deficit/hyperactivity disorder (ADHD)
Chemotherapy side effects
Chronic pain
Constipation
Fecal incontinence
Fibromyalgia
Headache
High blood pressure
Irritable bowel syndrome
Raynaud’s disease
Ringing in the ears (tinnitus)
Stroke
Temporomandibular joint disorder (TMJ)
Urinary incontinence
It’s noninvasive.
It might reduce or eliminate the need for medications.
It might enhance the benefits of medications.
It might help women who can’t take medication during pregnancy.
It helps people feel more in control of their health.
Risks
Biofeedback is generally safe, but it might not be appropriate for everyone. Biofeedback devices might not work properly on people with certain medical conditions, such as heart rhythm problems or certain skin conditions. Be sure to discuss it with your doctor first.
How you prepare?
You don’t need special preparation for biofeedback.
To find a biofeedback therapist, ask your doctor or another health care professional with knowledge of biofeedback therapy to recommend someone who has experience treating your condition. Many biofeedback practitioners are licensed in another area of health care, such as psychology, nursing, or physical therapy.
State laws regulating biofeedback practitioners vary. Some biofeedback practitioners choose to become certified to show
their extra training and experience in the practice.
During the procedure
During a biofeedback session, a therapist attaches electrical sensors to different parts of your body. These sensors might be used to monitor your brain waves, skin temperature, muscle tension, heart rate, and breathing. This information is fed back to you via cues, such as changes on a monitor, a beeping sound, or a flashing light.
The feedback teaches you to change or control your body’s reactions by changing your thoughts, emotions, or behavior. This can help the condition for which you sought treatment.
For instance, biofeedback can pinpoint tense muscles that are causing headaches. You then learn how to make deliberate physical changes in your body, such as relaxing specific muscles, to reduce your pain. The ultimate goal with biofeedback is to learn to use these techniques at home on your own.
Results
A typical biofeedback session lasts 30 to 60 minutes. The length and number of sessions are determined by your condition and how quickly you learn to control your physical responses. Biofeedback might not be covered by insurance.
If biofeedback is successful for you, it might help you control the symptoms of your condition or reduce the amount of medication you take. Eventually, you can practice the biofeedback techniques you learn on your own. Don’t stop the medical treatment for your condition, however, without consulting your care team.





One Comment